Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Prospective data confirming the role of anti-phosphatidylserine/prothrombin antibodies (aPS/PT) in the absence of other aPL tested by β2–glycoprotein I-depend assays are missing.
Methods: Since 2015 aPSPT was implemented as part of the routine testing in our SLE patients as part of the autoantibody screening. Patients with the revised criteria for SLE and fulfilling the following criteria were included in this study and prospectively followed-up.
- No previous TEs
- No concomitant anticoagulant therapy
- Negative tests aCL, anti-β2GPI (confirmed at least twice, at least 12 weeks apart)
All included patients were tested for aPS/PT at study inclusion. Positivity aPS/PT was defined as having at least two positive test results (IgG and/or IgM), at least 12 weeks apart.
Reports for objectively diagnosed TEs during follow-up had to include type, site, and the status of antithrombotic treatment at the time of event.
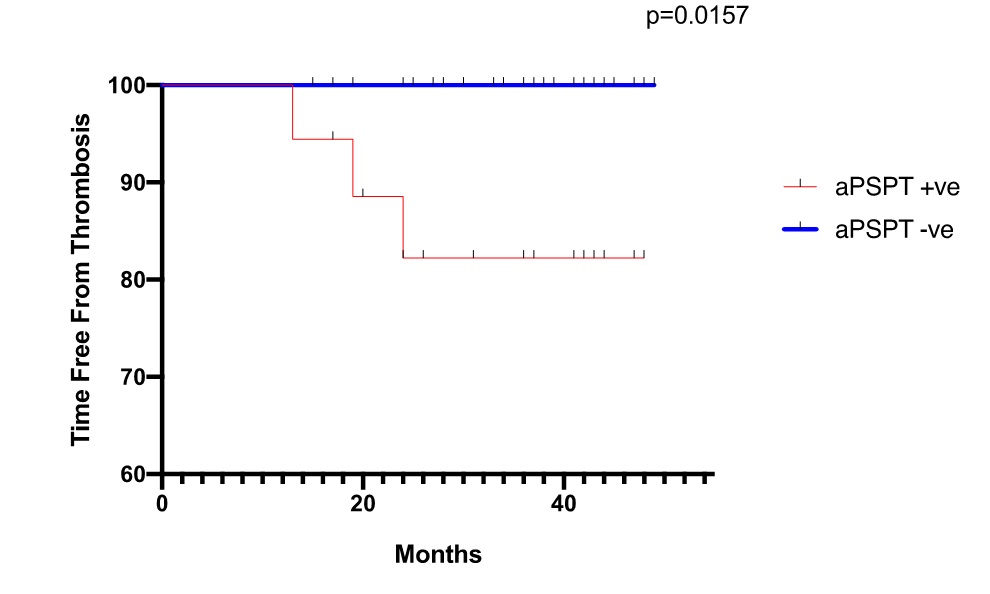
Results: This study included a total of 52 patients with SLE (42, 80.8% women). Of those 18 patients (34.6%) were found to be positive for aPS/PT (IgG and/or IgM). During a total follow-up of 238 years, there were 3 TEs (1.26% per year). The overall cumulative incidence of TEs was 5.8% after 2 years, being up to 16.7% when focusing on aPS/PT+ve patients (Figure 1). All the TEs events (2 cerebrovascular events and 1 thrombotic kidney microangiopathy) occurred in the aPS/PT+ve group. TEs not included among end-points were superficial thrombophlebitis in 2 subjects. No patient died and no pregnancy was recorded during the follow-up. The 3 patients with TEs were compared with the controls who did not have this complication. All patients tested negative for aΒ2GPI Domain 1 IgG.
aPS/PT was found to be associated with a trend in conferring an increased risk for TE (HR 12.9, 95% CI 0.70 to 236.74 p= 0.0851). When focusing on IgG aPS/PT we found that patients tested positive were at a significant higher risk for TEs (HR 19.6, 95% CI 1.0741 to 357.6416 p= 0.0446) when compared to controls.
Patients with TEs had a higher GAPSS when compared to those without, even if it failed to reach a statistically significance [6±2.64 Vs. 2±5.37, p=0.0971], probably due to sample size.
On multivariate analysis of considered variables (demographic factors, SLE features, arterial and venous risk factors), no factors was found to be statistically associated with the TEs.
Conclusion: Our prospective data validated previous retrospective studies demonstrating that aPS/PT, especially IgG, confers an increased risk for TEs in SLE patients.
To cite this abstract in AMA style:
Sciascia S, Radin M, Cecchi I, Rossi D, Roccatello D. A Prospective Study on the Incidence of a First Thrombo-embolic Event in Patients with Systemic Lupus Erythematosus and Anti-phosphatidylserine/prothrombin Antibodies [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/a-prospective-study-on-the-incidence-of-a-first-thrombo-embolic-event-in-patients-with-systemic-lupus-erythematosus-and-anti-phosphatidylserine-prothrombin-antibodies/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-prospective-study-on-the-incidence-of-a-first-thrombo-embolic-event-in-patients-with-systemic-lupus-erythematosus-and-anti-phosphatidylserine-prothrombin-antibodies/