Session Information
Date: Monday, November 13, 2023
Title: (1412–1441) Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster II: SpA
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Inflammatory cytokines can alter the way the central nervous system processes pain as shown in patients with rheumatoid arthritis. However, the relationship between TNFα inhibition and pain processing in individuals with psoriatic arthritis (PsA) has not been investigated.
The purpose of this study is to assess the feasibility of functional magnetic resonance imaging (fMRI) paradigm to estimate the respone to pain and the effect of treatment in PsA patients.
Methods: 6 patients with active PsA eligible to start a TNF inhibitor (TNFi) were included: 3 were naïve to biological disease modifying anti-rheumatic drugs and 3 were experienced. Four healthy subjects (HS) were also included. The physician selected a swollen and tender joint (affected joint) and a control joint in the contralateral hand (non-affected joint). Subjects were scanned in a 3.0T scanner at baseline (BL) and week 1 (W1) after starting treatment. First, the brain pain response was investigated pressing the non-affected joint followed by the affected joint. Each acquisition included 2 fMRI runs. The fMRI effect of pressure was represented for each subject individually, for each time point (p< 0.0001 uncorrected level, minimum extension 10 voxels). We provided a descriptive analysis of the differences in PsA patients brain response between BL and W1 and the clinical response evaluated by the percentage of improvement of Disease Activity in Psoriatic Arthritis (DAPSA) score and visual analogue scale pain (VASp) change.
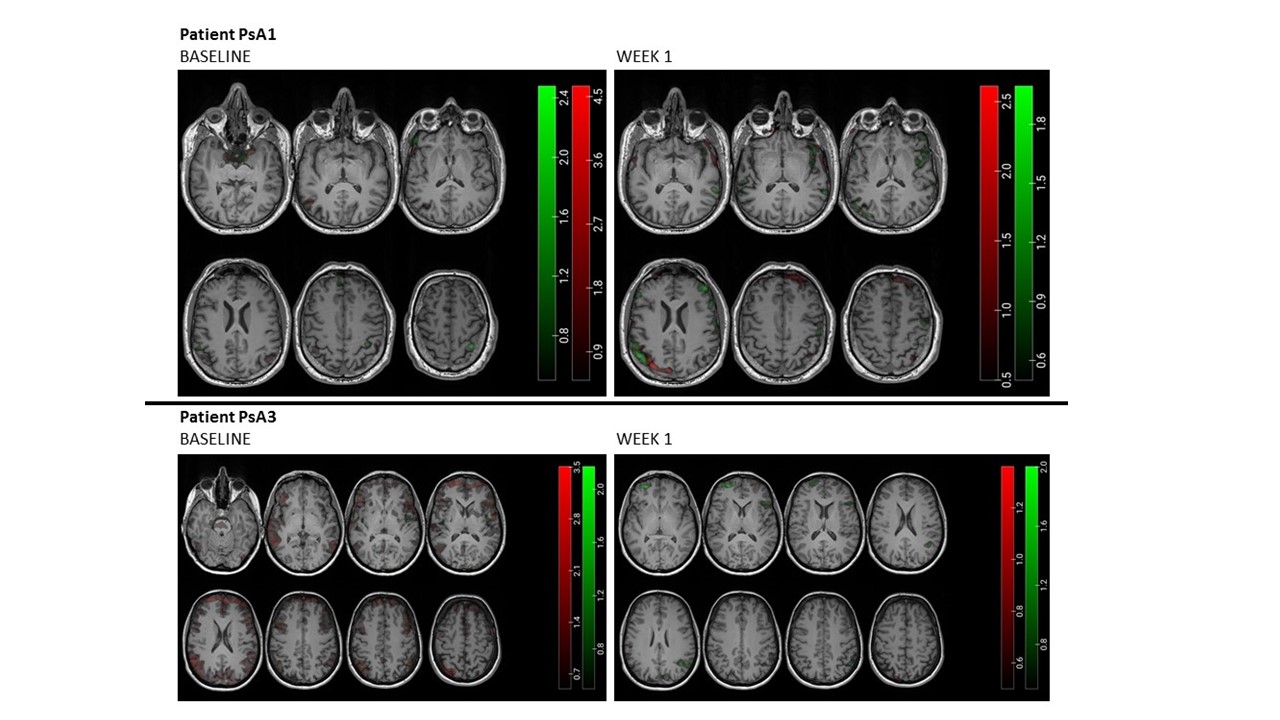
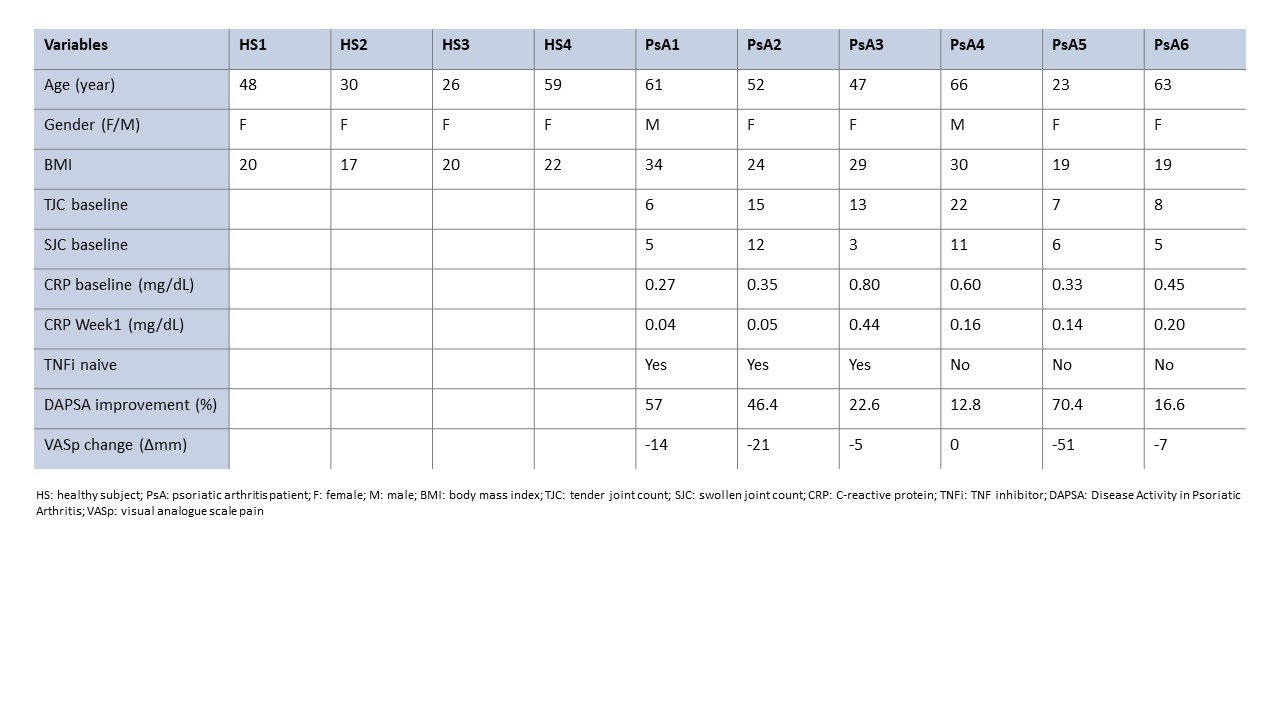
Results: All subject’s demographic characteristics and PsA patients’ clinical response are shown in Table 1. Brain response to pressure in HS produced activation in the sensory motor cortex, with more or less involvement of additional areas in the prefrontal, parietal and temporal cortex. In PsA patients with a higher treatment response (PsA 1, 2, 5), the brain response to pressure did not show any activation at BL whilst sensory motor cortex activation was seen at W1, with amygdala and insula activation in patients PsA 2 and 5 and prefrontal and frontal activity in patients PsA 1 and 2. In those with less response (PsA 3, 4, 6), the sensory motor cortex was activated at BL with little changes when evaluated at W1 (Fig. 1). No evident differences in brain response activation were observed between naïve and TNFi experienced patients.
Conclusion: The proposed fMRI paradigm seems to be a promising candidate to predict response to treatment with TNFi in PsA patients. Studies with more patients are needed to confirm our preliminary results.
Upper panel corresponds to a patient with clinical improvement (PsA1) and lower panel to a patient that did not respond (PsA3) at baseline (left column) and week 1 (right column).
Differences are observed in the sensorimotor cortex activation between patients: there is an increase in the activation after week 1 in PsA1 while PsA3 showed activation at baseline but not in week 1.
To cite this abstract in AMA style:
Espartal López E, Michelena Vegas X, Marsal Barril S, Rovira A, Pareto D, Erra Duran A. A Proof-of-concept Study Evaluating the Use of Functional Brain Magnetic Resonance Imaging in Assessing Treatment Response in Psoriatic Arthritis Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/a-proof-of-concept-study-evaluating-the-use-of-functional-brain-magnetic-resonance-imaging-in-assessing-treatment-response-in-psoriatic-arthritis-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-proof-of-concept-study-evaluating-the-use-of-functional-brain-magnetic-resonance-imaging-in-assessing-treatment-response-in-psoriatic-arthritis-patients/