Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Nearly half of systemic lupus erythematosus (SLE) patients will experience pregnancy complications. These complications include increased rates of prematurity, miscarriage, pre-eclampsia, and mortality. Maternal and fetal complications can be decreased with pregnancy planning. This retrospective chart review aimed to demonstrate the characteristics of pregnant SLE patients at a single institution and identify who cared for these patients in the perinatal period to determine where interventions to improve lupus pregnancy planning and management can be implemented.
Methods: This retrospective chart review identified adult patients diagnosed with SLE who were pregnant between October 2021 and October 2023. Patient data was obtained from the electronic medical record. Demographics, SLE manifestations, rheumatologic medications, and pregnancy/birth outcomes were extracted from all available healthcare systems. Next, patient appointments attended before and during pregnancy were reviewed. For patients not seen by a rheumatologist in the year before conception, specialists visited in the three years before pregnancy end were noted. Data was analyzed with descriptive statistics.
Results: Demographics
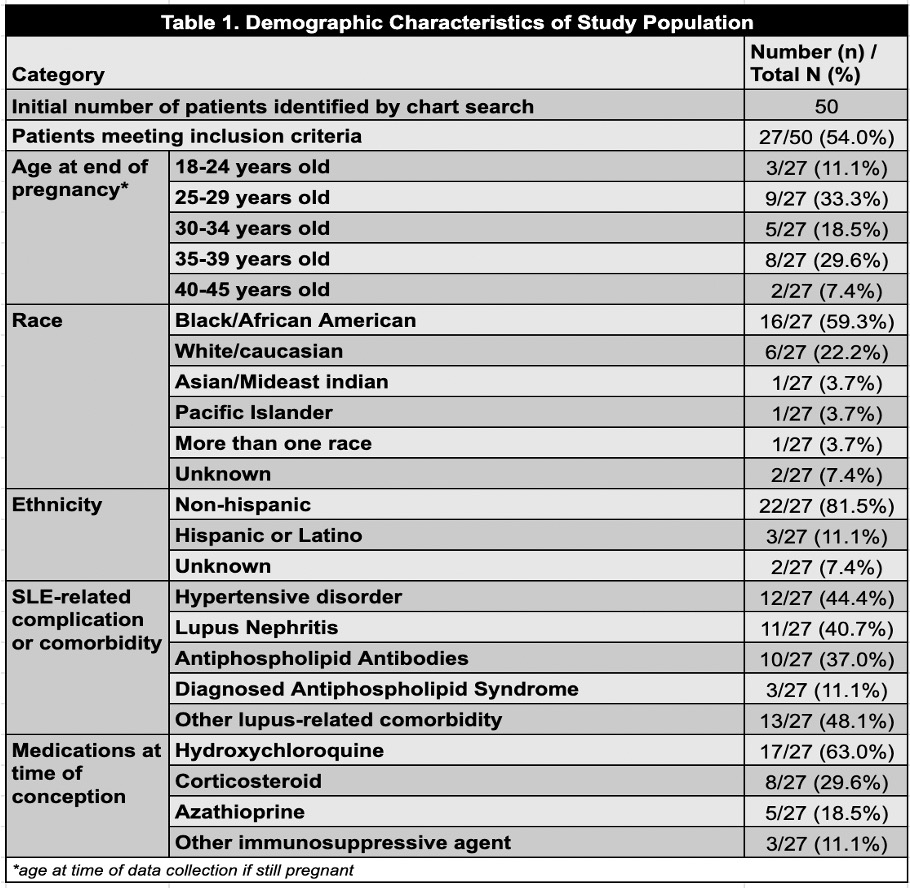
50 patients were initially identified. Those without a definitive diagnosis of SLE or pregnancy during the specified time frame (n=23) were excluded. Patients’ demographics were recorded (Table 1). While there was diversity across patient ages, the majority of patients were African-American (n=16, 59.4%) and non-Hispanic (n=22, 81.5%). The most common manifestations of SLE included hypertensive disorders (n=12, 44.4%), lupus nephritis (n=11, 40.7%), and positive antiphospholipid antibodies (n=10, 37.0%).
Patient Outcomes
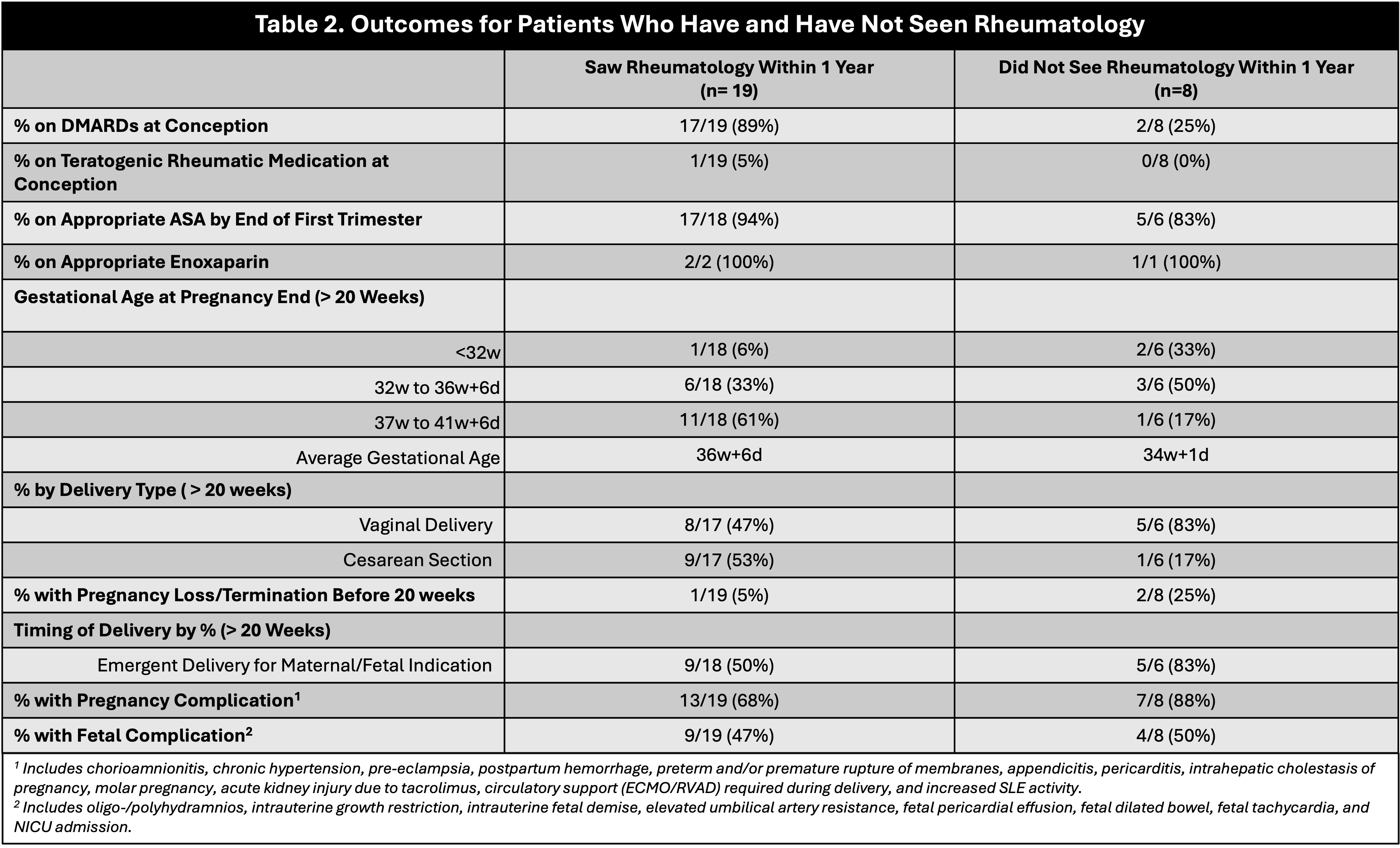
Differences were identified between patients who did and did not see a rheumatologist within one year before conception (Table 2). Patients seen by a rheumatologist were more likely to be on DMARDs, less likely to have pregnancy complications, and less likely to require an emergent delivery. For pregnancies carried beyond 20 weeks, the average gestational age at delivery was 36 weeks + 6 days for patients who were seen by a rheumatologist vs 34 weeks + 1 day for patients who were not.
Providers Seen and Opportunities for Intervention
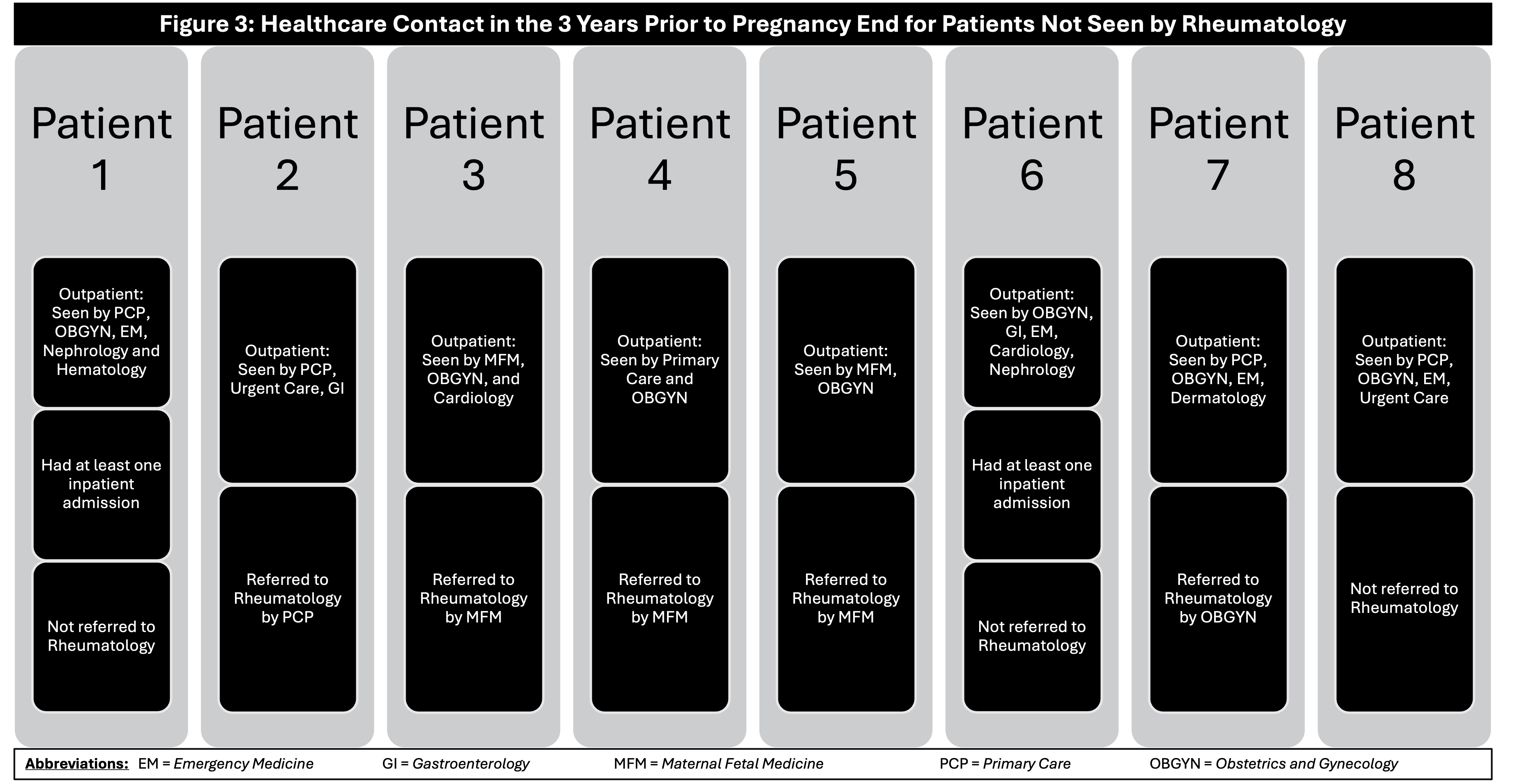
8 patients did not see a rheumatologist within one year of conception but did see other providers in the three years preceding pregnancy end (Figure 3). The providers who referred patients to a rheumatologist were primary care, obstetrics and gynecology, and maternal-fetal medicine.
Conclusion: This single-institution chart review demonstrated differences in pregnancy outcomes, including gestational age at delivery and percentage of emergent deliveries, between patients who did and did not see a rheumatologist in the year before conception. Larger chart reviews are needed to establish whether these differences are significant. Providers at our institution who did not refer patients with SLE to rheumatology to re-establish care included gastroenterology, cardiology, nephrology, and emergency medicine. These specialties present an institutional opportunity for interventions to improve perinatal outcomes for SLE patients.
To cite this abstract in AMA style:
Singh D, Faison M, Leavitt M, Clowse M, Edens C. A Pregnant Lupus Patient’s Journey: Single-Center Outcomes and Opportunities [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/a-pregnant-lupus-patients-journey-single-center-outcomes-and-opportunities/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-pregnant-lupus-patients-journey-single-center-outcomes-and-opportunities/