Session Information
Date: Sunday, November 10, 2019
Title: 3S075: Fibromyalgia & Other Clinical Pain Syndromes (827–832)
Session Type: ACR Abstract Session
Session Time: 2:30PM-4:00PM
Background/Purpose: In individuals with FM, regular participation in physical activity (PA) is associated with improvement of symptoms, daily physical functioning, and overall well-being. Given the importance but also the challenges associated with the initiation and maintenance of physical activity, it is imperative that therapeutic targets are identified to increase and maintain moderate level of PA.
Methods: This is a secondary data analysis of a 36-week randomized clinical trial to promote PA among patients with FM. Participants were randomized to 1 of 2 treatment arms: 6 phone-based motivational interviewing (MI) sessions or an equal number of FM self-management instructions.
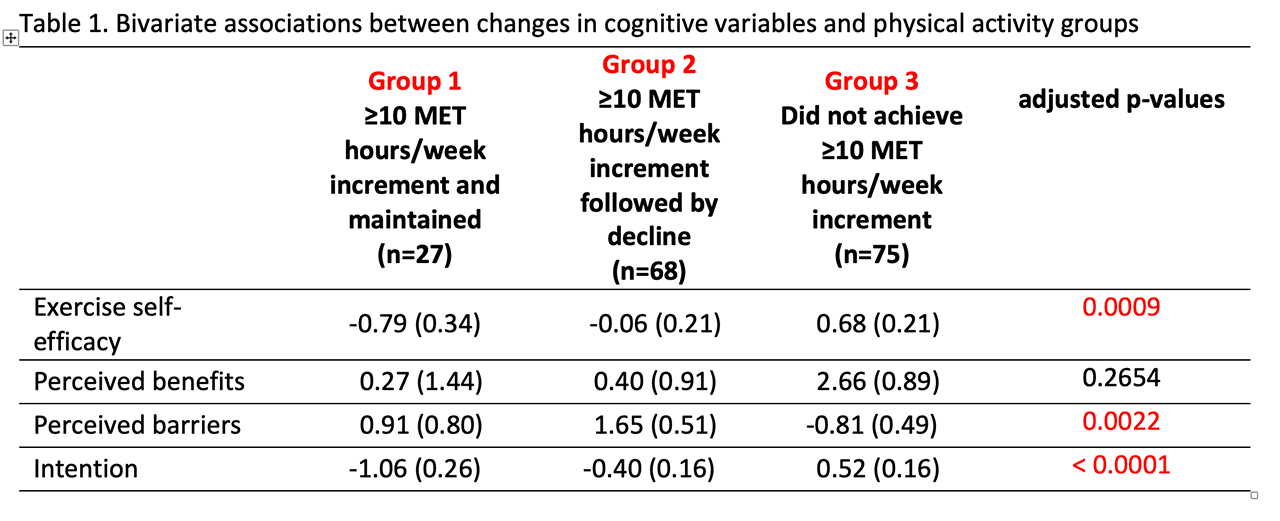
Changes in CHAMPS, a validated self-report measure of PA, were analyzed at each assessment period (baseline to week 12; week 12 to week 24; and week 24 to week 36). Based on CHAMPS, sustained PA was defined as an increase in moderate-vigorous PA (MVPA) of at least 10 MET h/week for ≥ 12 weeks. Using this threshold, three PA groups were defined based on subjects who: (Group 1) achieved a minimum increase of 10 metabolic equivalent (MET) hours/week that was subsequently sustained for at least 12 weeks; (Group 2) achieved a minimum increase of 10 MET hours/week that was not sustained for at least 12 weeks; and (Group 3) did not achieve an increase of at least 10 MET hour/week from baseline. Primary independent variables were baseline to week 36 changes in exercise self-efficacy, perceived benefits of PA, perceived barriers of PA, and intention to engage in MVPA. Initial analyses were performed using ANCOVA models to determine the association between cognitive variables and physical activity groups, adjusted for baseline values, and were performed using SAS v9.4. Controlling for treatment group assignment, path analyses were performed using M plus v7.31.
Results: For exercise self-efficacy, group 1 reported the largest improvement in exercise self-efficacy followed by group 2, and no improvement in group 3. For perceived barriers, groups 1 and 2 reported reductions in perceived barriers, while group 3 reported increased perceived barriers. For intention, groups 1 and 2 reported greater intention to engage in MVPA, while group 3 reported less intention. Change in perceived benefits were not significantly different among the 3 PA groups.
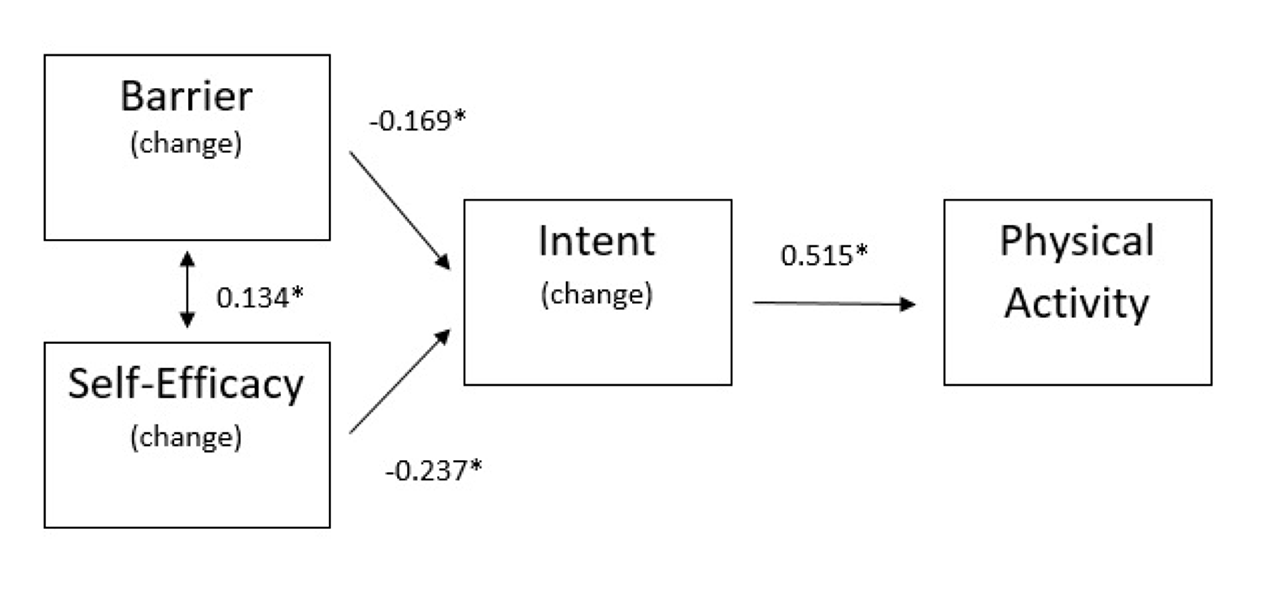
As shown in Figure 1 below, changes in perceived barriers and exercise self-efficacy influence intention to engage in PA, which in turn impacts changes in in the volume of PA. Perceived benefits of PA was not associated with either intention nor with physical activity. About 77% of the variance related to PA is explained by the model below.
Conclusion: When designing programs to promote PA in persons with FM, improving self-efficacy and resolving perceived barriers to exercise should be considered important therapeutic goals. Increasing awareness on the benefits of PA; however, may not elicit the desired PA behavior change.
To cite this abstract in AMA style:
Ang D, Kaleth A, Bush W. A Path Model Analysis of the Cognitive Determinants of Physical Activity Among Patients with Fibromyalgia (FM) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/a-path-model-analysis-of-the-cognitive-determinants-of-physical-activity-among-patients-with-fibromyalgia-fm/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-path-model-analysis-of-the-cognitive-determinants-of-physical-activity-among-patients-with-fibromyalgia-fm/