Session Information
Session Type: ACR Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Fragility fractures are associated with significant morbidity, mortality and healthcare costs, yet most fracture patients are neither evaluated nor treated for their underlying osteoporosis (OP). A Fracture Liaison Service (FLS) can improve OP treatment in patients with fragility fractures, including hip fractures. Our model uses a physician assistant Navigator to coordinate interdisciplinary care and provide a seamless transition between inpatient surgical care and outpatient OP management. The Navigator enhances patient education, facilitates communication amongst all providers, performs diagnostic evaluation as warranted, and initiates OP treatment.
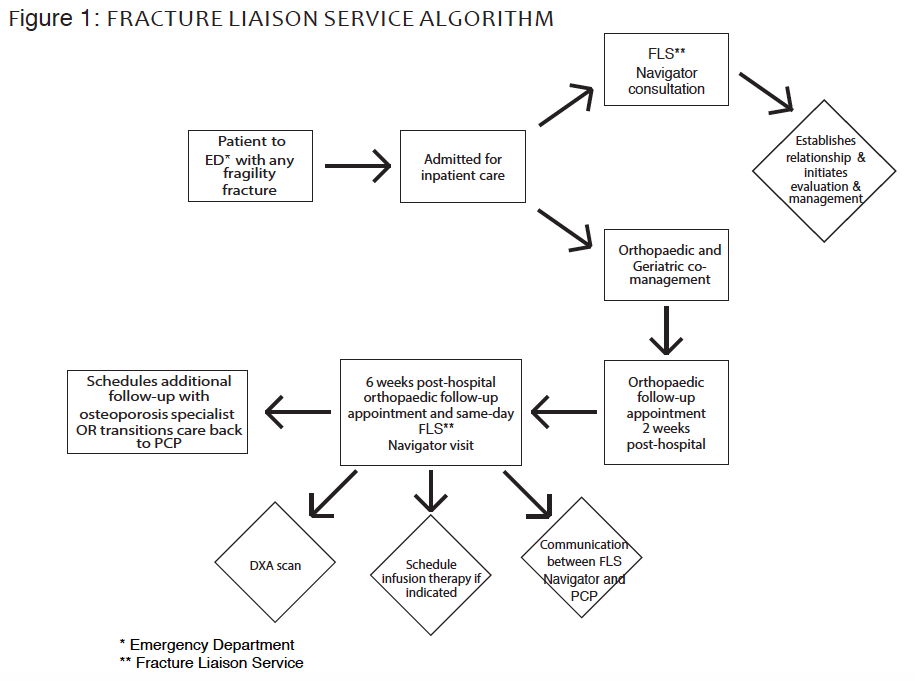
Methods: A patient-centered care algorithm (Figure 1) begins in the Emergency Department (ED), continues for inpatient hospital care with Geriatric, FLS and Orthopaedic co-management, and the FLS Navigator then transitions care to the outpatient setting (orthopaedic clinic). Communication between the FLS Navigator and patientÕs PCP occurs at each step.
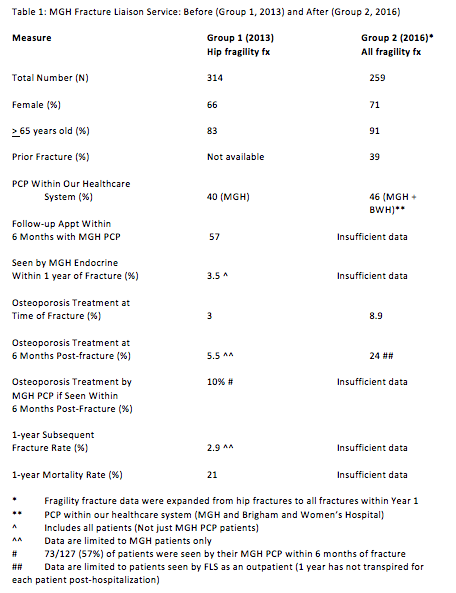
Results: A comparison of outcomes (Table 1) is made from 1/1/2013-12/31/2013 (Group 1, pre-MGH FLS) to 2/1/2016-1/31/2017 (Group 2, year 1 of MGH FLS). There were 314 hip fragility fractures in Group 1 (66% female, 83% age ≥ 65 years), and 259 fragility fractures in Group 2 (71% female, 91% age ≥ 65 years).
Of 314 Group 1 inpatients treated for a hip fragility fracture, 127 (40%) had a PCP in our health care system. Treatment was prescribed for 7 of 127 (5.5%) patients within 6 months of hip fracture and 11/314 (3.5%) were seen by an OP specialist within 1 year of fracture.
Of 259 Group 2 inpatients, 102 (39%) were seen as an outpatient by the FLS Navigator in the orthopaedic clinic or by a specialist in OP clinic. Of Group 2 patients, 68 (26%) declined a follow up appointment with the FLS Navigator and 32 (12%) did not keep the FLS outpatient appointment. Preliminary data reveal that 62 of 259 (24%) Group 2 patients were receiving OP therapy 6 months post-hospitalization, a greater than 4-fold increase compared to Group 1 (additional data not available for many Group 2 patients due to insufficient time since fracture).
Conclusion: The MGH FLS utilizes an innovative model to improve health outcomes, including morbidity, mortality and reduced healthcare costs, in a high risk population. Future goals include increasing the FLS scope to ensure all patients admitted with all fragility fractures are evaluated, improving 6-month treatment rates to >80%, expanding the FLS to fracture patients not requiring inpatient care, and using telemedicine to develop networks with regional hospitals.
To cite this abstract in AMA style:
Bolster MB, Cevallos S, Beyer L, Kronenberg HM, Leder B. A Model for Improved Management of Fragility Fractures: Navigating the Fracture Liaison Service [abstract]. Arthritis Rheumatol. 2017; 69 (suppl 10). https://acrabstracts.org/abstract/a-model-for-improved-management-of-fragility-fractures-navigating-the-fracture-liaison-service/. Accessed .« Back to 2017 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-model-for-improved-management-of-fragility-fractures-navigating-the-fracture-liaison-service/