Session Information
Date: Sunday, November 13, 2016
Title: Osteoporosis and Metabolic Bone Disease – Clinical Aspects and Pathogenesis - Poster
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporosis-related fractures contribute to increased morbidity and mortality in those affected and substantial economic burden to society. Effective screening for osteoporosis with fracture risk assessment tools (FRATs) is crucial to allow for needed preventive therapies. Electronic medical records (EMRs) present an important opportunity to identify patients at high risk for osteoporosis-related fractures. We compared the performance of four FRATs in identifying patients with osteoporosis by bone mineral density (BMD) T-score: The Veterans Affairs Fracture Absolute Risk Assessment Tool (VA-FARA), The World Health Organization’s Fracture Risk Assessment Tool (FRAX) based on patient-reported risk factors, the electronic FRAX (e-FRAX) which obtains inputs from the EMR, and the Osteoporosis Self-Assessment Screening Tool (OST). VA-FARA, FRAX, and e-FRAX are designed to identify fracture risk, which correlates with osteoporosis. OST is designed to identify osteoporosis.
Methods: We performed a cross-sectional analysis of all patients enrolled in the VA Salt Lake City Bone Health Team (BHT) from February 1, 2012 through February 1, 2013 who had a DXA. Patients were eligible for BHT intervention if they were males age 70+ or females age 65+. BMD scores were obtained by chart abstraction for each patient. Osteoporosis risk factors were obtained from a screening questionnaire which patients completed prior to DXA scan for calculation of FRAX. For VA-FARA and eFRAX risk factors were derived from the EMR. Clinical risk scores were then calculated and compared against the gold standard of DXA-based osteoporosis. Receiver operator characteristic (ROC) curves were plotted for each test and areas under the curve (AUC) were compared.
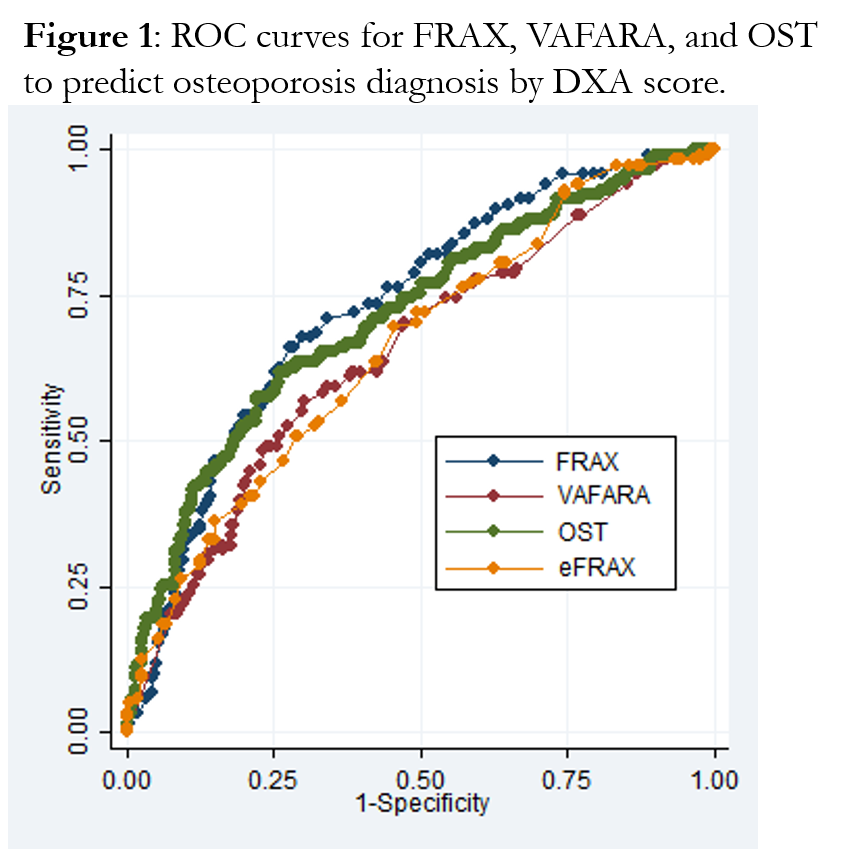
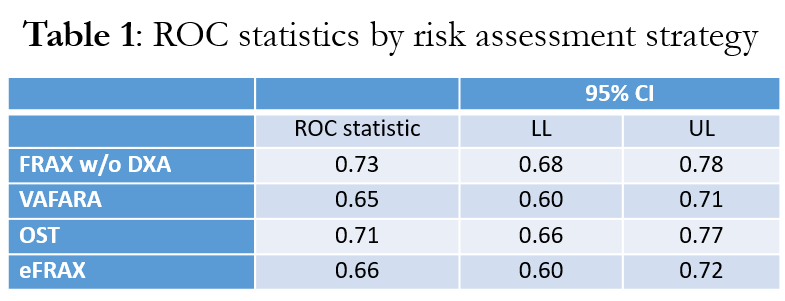
Results: A cohort of 473 patients met eligibility criteria (mean age 80.3 years, 98% male). Of these, 118 patients (25%) had osteoporosis as defined by DXA score < -2.5. There was no statistically significant difference between FRATs in identifying DXA-based osteoporosis. ROC curves are shown in figure 1. ROC statistics are shown in Table 1.
Conclusion: Our study suggests that FRATs perform similarly in identifying osteoporosis defined by BMD T-score among elderly Veterans. Electronic osteoporosis screening methods have a significant ease-of-use advantage by passively collecting risk factor data from the EMR. If these tools perform similarly for fracture outcomes as well, they could replace manual FRAX and thus improve efficiency in identifying individuals who should be sent for DXA scan to screen for osteoporosis.
To cite this abstract in AMA style:
Williams T, Lawrence P, Crook J, Nelson R, Lafleur J, Cannon GW. A Comparison of Electronic and Manual Fracture Risk Assessment Tools in Screening US Veterans at Risk for Osteoporosis [abstract]. Arthritis Rheumatol. 2016; 68 (suppl 10). https://acrabstracts.org/abstract/a-comparison-of-electronic-and-manual-fracture-risk-assessment-tools-in-screening-us-veterans-at-risk-for-osteoporosis/. Accessed .« Back to 2016 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-comparison-of-electronic-and-manual-fracture-risk-assessment-tools-in-screening-us-veterans-at-risk-for-osteoporosis/