Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose .Early data derived from small selected samples suggest that discoid lupus erythematosus (DLE) is negatively associated with renal involvement in patients with SLE. Recent findings from two large transversal studies are controversial, and the prognosis value of DLE on renal disease remains unclear. We used a longitudinal design to examine whether DLE onset protects against the development of LN in patients with systemic lupus erythematosus SLE from a large multiethnic Latin-American cohort.
Methods . We studied SLE patients enrolled in GLADEL, an inception longitudinal cohort from 34 centers in 9 Latin American countries. The main predictor was DLE onset, which was defined as physician-documented DLE that occurred before the diagnosis of SLE. The outcome was time from the diagnosis of SLE to LN during the followup. LN was defined by clinical or histological documentation of lupus glomerulonephritis or renal insufficiency secondary to LN. Kaplan-Meier analysis and Cox proportional hazard models were used to examine the association between DLE onset and time to LN.
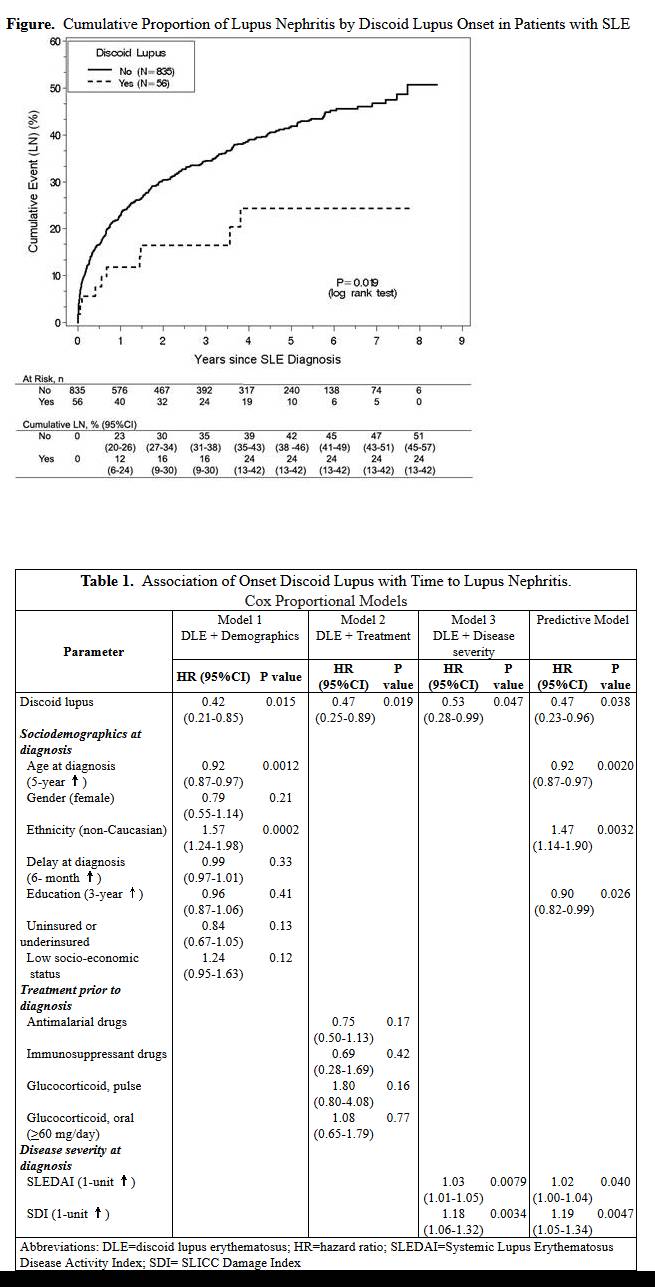
Results . We examined 891 GLADEL SLE patients at risk (91% females and 56% non-Caucasians). The mean age at SLE diagnosis and mean duration of follow-up were 30.8 years (SD 12.6) and 4.3 years (SD 2.3), respectively. Overall, 56 patients had DLE onset, and 329 developed LN during the followup. Among the LN group, only 10 (3.0%) had DLE onset, compared to 46 (8.2%) in the group that remained free of LN (p<0.0023). The cumulative proportion of LN at 1- and 5-year since SLE diagnosis was 12% and 24%, respectively in the DLE onset group, compared to 23% and 42% in those without DLE (p<0.0019) (Figure). Table 1 shows that DLE onset was negatively associated with time-to-LN after controlling for potential confounders. The final predictive model shows that the hazard ratio (HR) of LN in patients with DLE onset was 0.47 (95% CI 0.23–0.96) after controlling sociodemographic factors and disease severity at diagnosis.
Conclusion .Our data from the largest Latin-American SLE cohort indicate that the presence of DLE before the diagnosis of SLE protects against further LN, independently of other contributing factors such as age, ethnicity and SLE severity. These findings have relevant prognosis implications to SLE patients and their clinicians. Further studies are warranted to unravel the biological and environmental pathways implicated in the protective role of DLE against renal disease in patients with SLE.
Disclosure:
G. J. Pons-Estel,
None;
G. Bao,
GlaxoSmithKline,
2;
B. Pons-Estel,
None;
D. Wojdyla,
None;
V. Saurit,
None;
A. J. Alvarellos,
None;
F. Caeiro,
None;
E. I. Sato,
None;
E. R. Soriano,
None;
L. T. Costallat,
None;
O. Neira,
None;
A. A. Iglesias-Gamarra,
None;
G. Reyes Llerena,
None;
M. Cardiel,
None;
E. M. Acevedo-Vásquez,
None;
R. Chacon,
None;
C. M. Drenkard,
NIH,
2,
GlaxoSmithKline,
2.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/discoid-lupus-onset-and-decrease-risk-of-renal-disease-in-patients-with-systemic-lupus-erythematosus-data-from-a-large-latin-american-cohort/