Session Information
Title: Fibromyalgia, Soft Tissue Disorders, Regional and Specific Clinical Pain Syndromes: Clinical Focus
Session Type: Abstract Submissions (ACR)
Background/Purpose: Although criteria exist for fibromyalgia (FM) diagnosis, little is known about how FM diagnosis is applied and understood by physicians and patients in the US population. The 2012 National Health Interview Survey (NHIS) is the largest US population-based health survey. We examined the relation between self-reported physician FM diagnosis, polysymptomatic distress (PSD), demographics and selected symptoms captured in the NHIS.
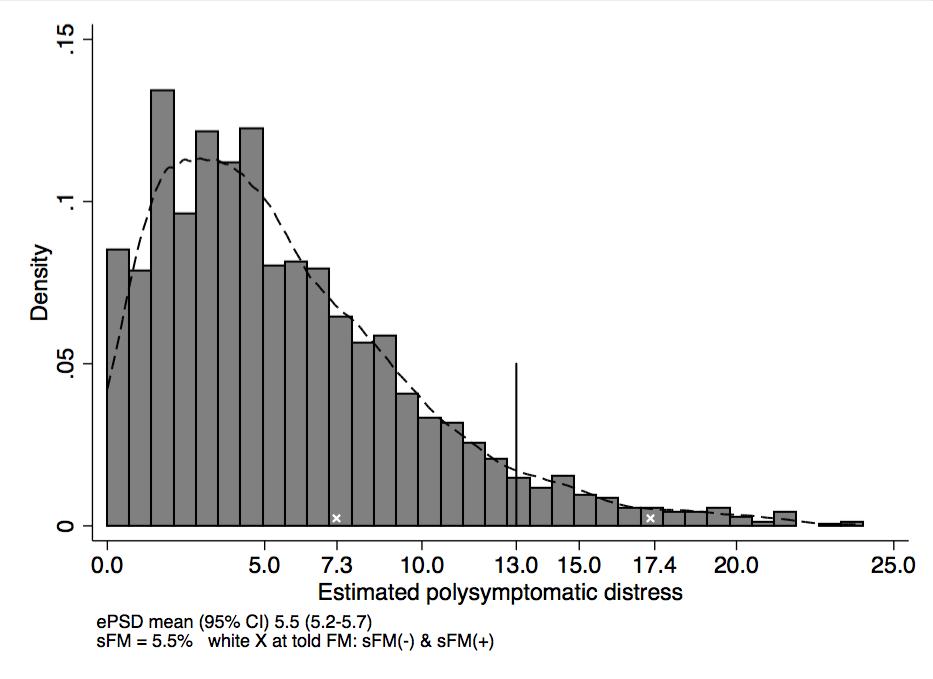
Methods: The NHIS asked participants about receiving a FM diagnosis from a physician along with questions about joint pain and somatic symptoms. We developed NHIS FM/PSD definitions by administering germane NHIS questions and the modified 2010 ACR criteria to 415 consecutive rheumatology patients in 2 clinics. After applying these definitions to the NHIS, we estimated a PSD score (ePSD) and set a surrogate FM diagnosis (sFM) at ePSD ≥ 13. Because of differences in questions and administration between the ACR criteria and the NHIS, the current data should be considered approximate.
Results: The ePSD distribution in the NHIS is shown in Figure 1. Using population derived survey weights in a sample of 2,680 participants , 4.8% reported being told they had FM (FM+); 5.6% met the criteria for sFM (sFM+).Table 1 shows the subjects stratified by told FM and sFM status. Of FM (+) subjects, 83.0% were sFM (-). Subjects that were FM (+) but sFM (-) were similar to the non-FM population but with modest increases in ePSD, not working, and lifetime depression (Table 1). In addition, they were generally white (82.1%) and female (91.0%). FM (-) but sFM (+) subjects were less often white (69.1%) or female (66.8%). Women were more likely to report being told they had FM (odds ratio 9.6) but not as likely to meet sFM criteria (odds ratio 2.1).
Conclusion: More than 80% of subjects in NHIS who report being told by physicians they have FM do not satisfy sFM criteria. Among these subjects, more are female and non-minorities than in those satisfying sFM criteria. In addition, FM (+) individuals are generally indistinguishable from the non-FM population (FM -), but are less likely to be employed and more likely to report functional limitations and a lifetime history of depression. The cause for over-diagnosis is likely multi-factorial, but may include physician misdiagnosis, access to health care, personal beliefs, and socio-cultural ideas about FM engendered by academic and industry messaging. Regardless, our current medical approach to FM/PSD results in 3.9% of minimally symptomatic Americans reporting themselves labeled as “sick”. These results have important public health implications.
|
Group |
Category % |
Mean ePSD score |
% White |
% Female |
% High School graduate |
% Not working |
% Functional limitations |
% Lifetime depression |
|
Not told FM, Not sFM |
93.3 |
4.7 |
75.8 |
51.6 |
75.8 |
47.1 |
63.4 |
21.9 |
|
Told FM, Not sFM |
3.9 |
7.3 |
82.1 |
91.0 |
82.1 |
73.5 |
73.7 |
42.1 |
|
Not told FM, +sFM |
1.9 |
15.7 |
69.1 |
66.8 |
69.1 |
73.7 |
91.7 |
63.2 |
|
Told FM, +sFM |
0.8 |
17.4 |
89.6 |
83.0 |
89.6 |
78.4 |
100.0 |
58.2 |
Disclosure:
B. Walitt,
None;
R. Nahin,
None;
R. S. Katz,
None;
M. J. Bergman,
None;
F. Wolfe,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/most-patients-diagnosed-with-fibromyalgia-by-physicians-do-not-have-fibromyalgia-the-2012-national-health-interview-survey-fibromyalgia-study/