Session Information
Session Type: Abstract Submissions (ACR)
Background/purpose: To assess clinical outcomes including pulmonary function and radiographic imaging in patients with ILD and the antisynthetase syndrome who were treated with Rituxan (RTX)
Methods: We retrospectively identified all patients at one institution with the antisynthetase syndrome who presented with ILD and were treated with RTX. Data regarding demographics, serologic status, muscle disease, concomitant steroid use, pulmonary function testing and chest CT scans were assessed before and after the use of RTX. Serial assessments with PFTs were performed using standardized methods. Two radiologists independently evaluated axial chest CT scans using a standardized scoring system ( Oda et al. Respiratory Research 2014, 15:10) and made a subjective assessment of the type of ILD pattern at 0 and 6 months and the scores of the two radiologists were averaged.
Results: 12 patients were identified who were treated with RTX for the anti-synthetase syndrome. Anti-synthetase antibodies were identified in all patients (5 PL-12, 4 Jo-1, 3 PL-7). 11 patients (92%) were females and the mean age was 54. Three patients (25%) had been smokers. The diagnosis of antisynthetase syndrome followed the diagnosis of ILD in 8 patients (67%) by a mean of 4.5 years. 7 of the patients had myositis. In 9 cases (75%), the principal indication for use of RTX was recurrent or progressive ILD due to failure of other agents. Mean time to initiation of RTX after identification of ILD was 5.4 years. One patient discontinued RTX in this time due to anaphylaxis. One patient proceeded to lung transplant, and 2 patients had serious gastrointestinal complications requiring surgery but subsequently resumed RTX.
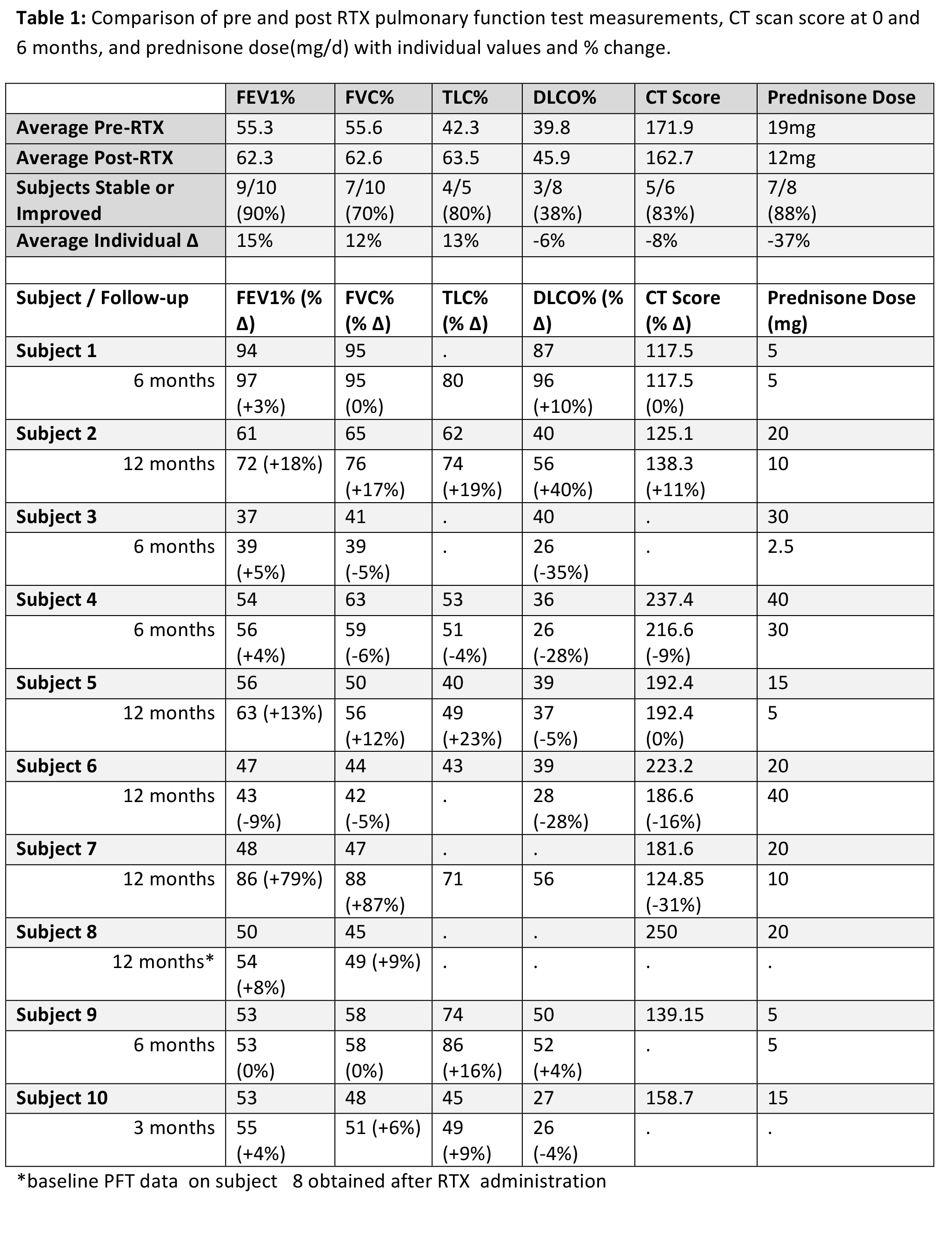
Comparing pre and post RTX PFTs at 3-12 months for the 10 patients with adequate follow-up, FVC% and TLC% were stable or improved in 70% and 80% of subjects, and DLCO% increased in 38% [Table 1]. The average individual change was 12%, 13%, and -6%, respectively. CT score was stable or improved in 83% of subjects where followup CT was available. Eight CTs were consistent with non specific interstitial pneumonia (NSIP) and 2 had components of both cryptogenic organizing pneumonia (COP) and NSIP. Steroid dose decreased in 88% of subjects with an average decrease in dose of 6mg.
Conclusions: Use of RTX was well tolerated in the majority of patients who had ILD and the anti-synthetase syndrome. Stability or improvement in pulmonary function or CT imaging was seen in most patients. RTX may play a therapeutic role in patients with ILD associated with the antisynthetase syndrome and further clinical investigation is warranted.
Disclosure:
T. Doyle,
None;
J. Osorio,
None;
E. Nilo DeMagaldi,
None;
R. Madan,
None;
F. Cabral,
None;
I. Rosas,
None;
P. Dellaripa,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/assessment-of-the-effect-of-rituximab-in-the-treatment-of-interstitial-lung-disease-associated-with-the-antisynthetase-syndrome/