Session Information
Title: Rheumatoid Arthritis - Clinical Aspects (ACR): Comorbidities, Treatment Outcomes and Mortality
Session Type: Abstract Submissions (ACR)
Background/Purpose: Rheumatoid arthritis (RA) is a multisystem inflammatory disease characterized by a symmetric, destructive polyarthritis. Interstitial lung disease (ILD) is an extra-articular manifestation that occurs in 7.7% of RA patients and confers a poor prognosis. The anti-citrullinated peptide (anti-CCP) antibody has a specificity of greater than 90% for RA and is associated with worse articular outcomes. Four studies have evaluated the association between anti-CCP and ILD in RA patients with contradictory results. Furthermore, there are no published observations of an association between the extent of the anti-CCP titer elevation and the prevalence of ILD. The objective of this study is to determine whether the anti-CCP titer is associated with the prevalence of ILD in patients with and without RA.
Methods: A chart review was performed of all adult patients with anti-CCP testing between January 1, 2007 and December 31, 2012 at a single academic hospital. Patients were excluded if they had any of 12 other exposures or conditions known to cause ILD. Patients meeting inclusion criteria were divided into four groups based on anti-CCP titers: 0-4 U/mL (negative titer), 5-149 U/mL (low titer), 150-299 U/mL (moderate titer), and 300 U/mL or greater (high titer). Charts were reviewed to determine a diagnosis of RA by a rheumatologist or American College of Rheumatology (ACR) 2010 criteria, a diagnosis of ILD by imaging, relevant laboratory analysis, and treatment of RA. Fisher’s exact test and logistic regression were used to compare the prevalence of ILD in the anti-CCP titer groups and to adjust for potential confounders.
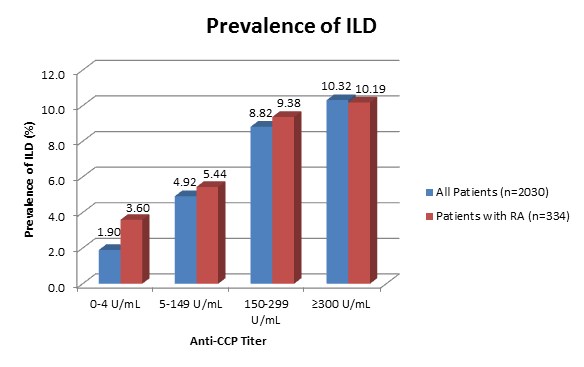
Results: 2,030 patients met inclusion criteria, and 334 of these patients were diagnosed with RA by a rheumatologist or 2010 ACR criteria. Among all patients tested for anti-CCP, a progressively higher prevalence of ILD was associated with each anti-CCP titer group (p<0.0001) (Figure 1). However, the association was diminished when adjusting for age, C-reactive protein (CRP), tobacco use, and a diagnosis of RA (odds ratio: 1.18, 95% confidence interval: 0.78-1.78). In patients diagnosed with RA, there was a similar progression in the prevalence of ILD as anti-CCP titers increased, although this finding did not achieve statistical significance (p=0.18).
Conclusion: An increasing prevalence of ILD was observed in patients with higher levels of anti-CCP titers, regardless of a diagnosis of RA. However, additional factors, particularly age and disease activity represented by CRP, may influence these findings. To our knowledge, this is the first study to evaluate the relationship of increasing anti-CCP titers and ILD prevalence. Larger investigations are essential to better define the role of anti-CCP in the development of ILD and to determine whether higher anti-CCP titers further augment the risk of developing ILD.
Disclosure:
C. Correia,
None;
M. R. Bussey,
None;
B. Panico,
None;
R. Guo,
None;
R. A. Ostrowski,
None.
« Back to 2014 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/anti-citrullinated-peptide-antibody-titers-and-the-prevalence-of-interstitial-lung-disease-in-patients-with-and-without-rheumatoid-arthritis/