Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Rheumatoid arthritis (RA) patients have increased prevalence of carotid atherosclerosis, especially plaque formation, which has been associated with inflammatory burden in a previous study. We sought to investigate the risk factors of carotid atherosclerosis progression and cardiovascular events (CVE) in RA patients in a prospective cohort study.
Methods: Progression of carotid atherosclerosis, determined by carotid ultrasound and the incidence of CVE were investigated in a prospective KARRA cohort. All patients and healthy controls were prospectively followed up for 5 y ears or until deaths. Conventional CV risk factors, RA disease activity and severity markers, medication histories, and calculated areas under the curve of erythrocyte sedimentation rate (ESR-AUC) for 2 years follow-up were analyzed.
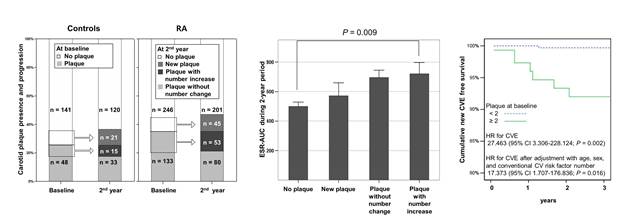
Results: Mean age and female frequency of RA patients were not different compared with those of healthy controls (54 ± 12 vs. 55 ± 12, 81.6 vs. 78.8%, respectively). The number of carotid plaques increased more rapidly in RA patients compared with controls during 2 years of follow-up (0.3 ± 0.7 and 0.2 ± 0.6, respectively, P = 0.030). Frequencies of new carotid plaques among subjects without plaque at baseline were not different between RA patients and controls. However, subjects with increased number of plaques who had plaques at baseline were more frequent in RA patients compared with controls (OR 3.086 [95% CI 1.518-6.276; P = 0.002]). RA patients with increased number of plaques who had plaques at baseline were significantly associated with modified health assessment questionnaire, tender and swollen joint counts, DAS28, methotrexate (MTX) dose, and ESR-AUC for 2-year period. In a multivariate analysis, tender joint count 68 (OR 1.129 [95% CI 1.025-1.243; P = 0.014]), ESR-AUC (OR 1.001 [95% CI 1.000-1.002; P = 0.022]), and MTX dose (OR 1.424 [95% CI 1.103-1.839; P = 0.007]) were independently associated with these patients. During the 2-year period, CVE occurred in seven (1.7%) among RA patients compared with one (0.5%) among controls. In RA patients, higher number of carotid plaques was significantly associated with CVE (P = 0.001). Furthermore, the incidence of CVE was 4.1% among patients with plaque, compared with 0.4 % among patients without plaque (RR 10.859 [95% CI 1.294-91.095; P = 0.011]). In a Cox regression model, two or more carotid plaque presence predicted CVE in RA patients during 2-year period (hazard ratio 27.463 [95% CI 3.306-228.124; P = 0.002]).
Conclusion: These prospective data suggest that the incidence of CVE depends on by baseline carotid plaques, the progression of which is strongly associated with time-integrated inflammatory burden in RA patients.
Disclosure:
C. H. Im,
None;
S. H. Kwon,
None;
J. S. Eun,
None;
N. R. Kim,
None;
E. J. Nam,
None;
Y. M. Kang,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammatory-burden-predicts-carotid-plaque-progression-and-subsequent-cardiovascular-events-in-rheumatoid-arthritis-the-2-year-prospective-cohort-study/