Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The risk of osteoporotic fracture is known to be high in RA. Yet less is known about RA related predictive factors for this complication & its associated economic burden.
Methods: The Early RA Study (ERAS, 9 centres) recruited 1465 DMARD naïve patients between 1986-1998 & the Early RA Network (ERAN, 23) 1236 patients, 2002-2012. Standard clinical, radiological & laboratory measures were performed yearly for 25 & 10yrs (median 10 & 3yrs respectively). Major comorbidities & in-patient hospital episodes were recorded yearly, including fracture sites & orthopaedic surgery. Clinical databases were supplemented & validated with national databases: National Joint Registry (data available 2003-2011), Hospital Episode Statistics (1997-2011) & National Death Register (1986-2011). Treatment regimens followed guidelines of the era, mainly conventional DMARD therapies, +/- steroids, & latterly biologics.
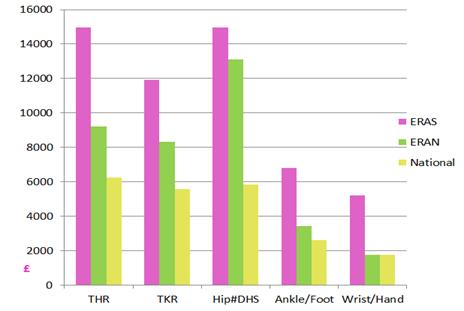
Results: A total of 178 (6.6%) patients had 182 fractures, the majority hip (42%), wrist fractures (17.5%), & vertebrae (12%). Other fractures (28.5%) included the distal forearm, foot & ankle. 13 hip fractures resulted in total hip replacements & 57 in dynamic hip screw surgery. None of the procedures were complicated by death in the postoperative period, although hip & vertebral fractures were recorded as contributory causes of death in 12 & 2 respectively. The average length of stay (LoS) varied across procedures, with hip fractures incurring the longest LoS (median 15days in the first decade of the study, 8days in the last). The LoS appeared to drive costs (graphs to demonstrate this). Compared to national data, both LoS & consequently costs were higher in RA patients sustaining osteoporotic fractures, compared to other RA-related intervention or other orthopaedic surgery undertaken nationally by non-RA patients (figure 1). The median time from baseline to hip fracture was 8yrs (IQR 5-15). In hip fracture patients, the mean number of all & major comorbid conditions was increased (3.7 & 1.4) compared to non-fracture (1.8 & 0.9, p <0.001), & survival reduced (48% vs 20%, p<0.0001). Aside from traditional risk factors (age, gender), baseline & 1yr disease activity measures were identified as potential predictors: erosions (OR 2.4, 95%CI 1.4-4.0), high rheumatoid factor (OR 1.7, 95%CI 1.1-2.9), high HAQ (OR 1.7, 95%CI 1.1-2.9), high ESR (OR 1.9, 95%CI 1.1-3.1), low haemoglobin (OR 1.99, 95%CI 1.2-3.1). Steroid use predicted higher risk for fracture: OR 2.7, 95% CI 1.1-6.5.
Conclusion: RA over 25yrs was complicated by osteoporotic fracture in 6.6% patients, mainly hip fractures, which were not a late complication of RA. Most required major orthopaedic surgery, & were associated with comorbidity & reduced survival, as well as high costs. Markers of active disease were associated with a higher risk of fracture, highlighting the need for more active therapies for RA control & bone protection.
Figure 1:
Disclosure:
E. Nikiphorou,
None;
L. Carpenter,
None;
J. Dixey,
None;
P. Williams,
None;
P. D. Kiely,
None;
D. Walsh,
None;
R. Williams,
None;
A. Young,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/osteoporotic-fracture-and-post-operative-clinical-and-cost-outcomes-in-rheumatoid-arthritis-results-from-two-uk-inception-cohorts/