Session Information
Title: Systemic Lupus Erythematosus - Clinical Aspects I - Renal, Malignancy, Cardiovascular Disease
Session Type: Abstract Submissions (ACR)
Background/Purpose: Proteomic analysis of urine samples, from patients with active lupus nephritis (LN)1-2 and from animal model of LN3 has led to identification of Prostaglandin D synthetase (PGDS) as a potential biomarker in LN. The levels were increased in patients with active LN as compared to inactive LN1.There is no longitudinal study available in patients with active LN to see its relationship with renal activity.
Methods: Patients fulfilling ACR criteria for diagnosis of SLE were included and categorized into active LN (ALN), active non renal disease (ANR) and inactive disease (ID). Urine was collected in the morning and stored after centrifugation. Patients with pregnancy or infection were excluded. Urine samples from 19 healthy young females were included as control. 25 patients with active lupus nephritis were followed up 3 monthly and urine samples were analyzed at 6, 9 and 12 months. Patients who had worsening renal disease at 3 months had sample analyzed at 3 months also. Urinary PGDS (uPGDS) was measured by ELISA using commercial kit. All values were normalized to urinary creatinine excretion.
Results: A total of 28 patients with ALN, 15 patients with ANR, 6 patients with ID and 19 healthy controls were included in cross-sectional study. Among the 49 patients, there were 46 females. Mean age was 27.8(SD 9.5) years. The median SLEDAI in ALN was 20(6-32), in ANR was 9(4-18) and in ID was 3(0-4). In patients with ALN, the median renal SLEDAI was 10(4-16). The class of LN was II in 4, III in 11, IV in 6, V in 3 and in 4 patients biopsy could not be done.
In cross-sectional study, the median uPGDS excretion was higher in patients with ALN (61.85 ng) as compared to healthy controls (14.17ng; p<0.001), ANR ( 21.31ng; p=ns) and ID (5.62 ng; p<0.005). uPGDS had good correlation with renal SLEDAI (r=0.403; p=0.006) and total SLEDAI (r=0.406; p=0.007).
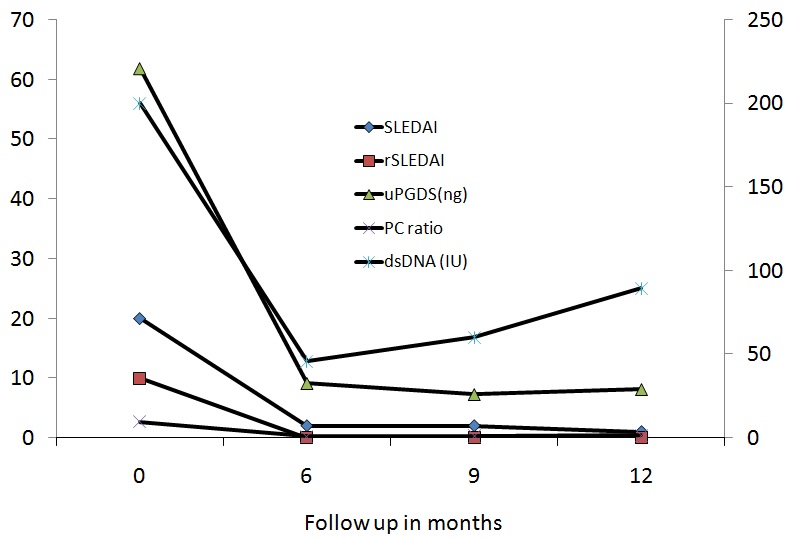
In longitudinal study of 28 patients with ALN, 25 patients had completed 6 months, 20 patients 9 months and 13 patients 12 months follow-up. uPDGS had excellent correlation with SLEDAI, rSLEDAI and urinary protein creatinine ratio over time. The median values are shown in the line diagram below at 0, 6, 9 and 12 months.
One patient with class IV nephritis had no response at 3 months with rise in serum creatinine. Her urine sample at 3 months showed a marked rise in uPGDS (41.89 to 390.85ng). She was treated with Rituximab but developed ESRD at 6 months.
The only patient who showed a significant rise in uPGDS at 9 months (baseline: 13.9: 6 months: 10.9: 9 months 47.96 ng) relapsed at 11 months.
Conclusion: uPGDS is a good marker of lupus activity. uPGDS is partly serum derived3 as its levels are higher in patients with ANR disease than ID. Its levels are higher in nephritis and can be used to monitor renal activity. It may be a potential marker to predict relapse.
References: 1J Prot 2012;75:3240-7.2Ped Res 2009;65:530-6.3J Immunol2010;184;2183-93.
Disclosure:
R. Gupta,
None;
A. Yadav,
None;
R. Misra,
None;
A. Aggarwal,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/urinary-prostaglandin-d-synthetase-as-a-biomarker-of-lupus-nephritis-activity-one-year-longitudinal-study/