Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Fatigue and exercise intolerance affect over 90% of patients with SLE, often persisting despite inactive disease and disrupting quality of life. Yet, the underlying mechanism remains poorly defined, and treatment options are limited. We report a detailed evaluation and therapeutic response in a series of ten women with SLE and disabling fatigue and exercise intolerance, identifying preload deficiency as a potential and treatable contributor.
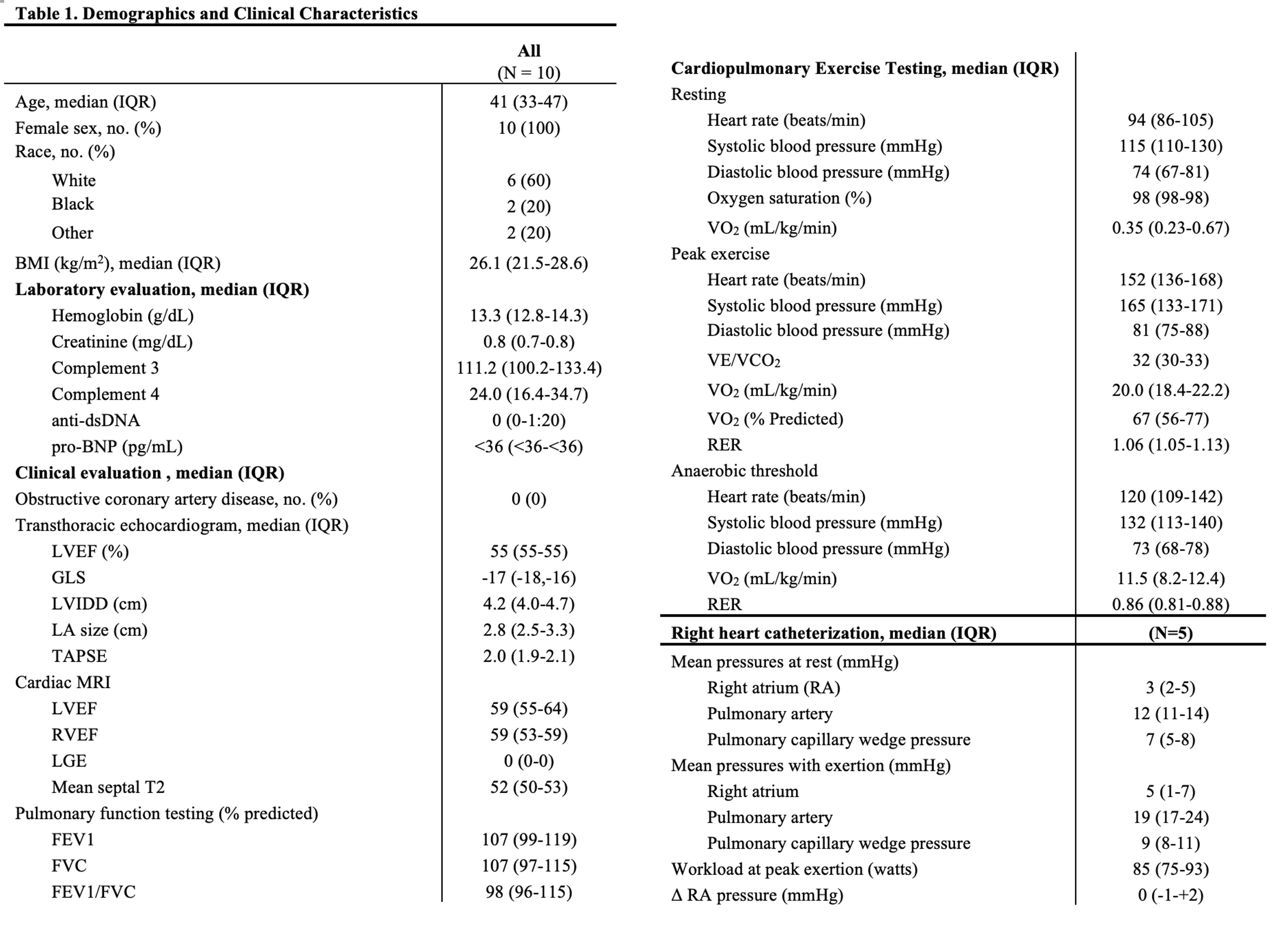
Methods: A prospective cohort study of ten women with SLE who experienced exercise intolerance and fatigue was conducted as part of the Hopkins Lupus Cohort. All patients underwent extensive cardiopulmonary evaluation, including laboratory tests, transthoracic echocardiography (TTE), cardiac MRI, continuous cardiac monitoring, coronary CT, quantitative autonomic testing (QAT), and cardiac pulmonary exercise testing (CPET). A subset of these patients underwent right heart catheterization (RHC) with exertion.
Results: The median age was 41. All patients had no anemia, renal, or pulmonary dysfunction. TTE, cardiac MRI, continuous cardiac monitoring, and coronary CT were unremarkable, indicating no structural, coronary, or conduction abnormalities. QAT identified postural orthostatic tachycardia syndrome (POTS) in 2 patients. However, all demonstrated impaired aerobic capacity (peak VO₂ < 80% predicted) on CPET, with low anaerobic thresholds and elevated resting heart rates, indicating cardiovascular limitation to exercise. Jugular venous pressure (JVP) was < 5 cm H₂O in all cases, suggesting preload deficiency, a condition of inadequate augmentation of right-sided filling pressures during exertion. To confirm, five patients underwent RHC with exertion, all demonstrating preload deficiency defined as failure to increase right atrial pressure with exercise (ΔRAP< 5.5). Pro-BNP was undetectable in all, consistent with inadequate right atrial filling and suggesting its potential utility as a biomarker.Patients were advised to increase fluid (128 oz/day) and sodium intake ( >5g/day) and use compression garments. Ivabradine was introduced in a subset of patients with persistent symptoms, high resting heart rates, marked exertional tachycardia, or limited fluid/sodium tolerance. All patients reported significant symptomatic improvement. One patient, previously nearly bed-bound, returned to school and completed a doctoral degree.
Conclusion: Reduced peak VO₂ and anaerobic thresholds have been described in SLE. Our findings suggest that preload deficiency—a reversible cardiovascular abnormality—may underlie this impairment in selected patients, offering a previously unrecognized but treatable cause of exercise intolerance. Undetectable pro-BNP may serve as a biomarker of preload deficiency in this population, warranting further study. Recognition of this phenotype may enable effective, low-risk interventions and offer a mechanistic target for future studies aimed at defining the prevalence and pathophysiology of preload deficiency in SLE.
To cite this abstract in AMA style:
Kim Y, Ismail P, Petri M, Lee J, Adamo L, Fava A. Preload deficiency as a treatable cause of fatigue and exercise intolerance in SLE [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/preload-deficiency-as-a-treatable-cause-of-fatigue-and-exercise-intolerance-in-sle/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/preload-deficiency-as-a-treatable-cause-of-fatigue-and-exercise-intolerance-in-sle/