Session Information
Date: Tuesday, October 28, 2025
Title: (2377–2436) Systemic Lupus Erythematosus – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Cutaneous lupus erythematosus (CLE) is an autoimmune disease primarily manifesting in skin that can significantly impact patients’ quality of life. Current understanding of the direct healthcare cost of CLE is limited. This study was conducted to understand the direct costs of CLE compared with psoriasis, atopic dermatitis (AD), and a general patient population.
Methods: Data from January 1, 2016, to December 31, 2023, were extracted from the Optum® de-identified Clinformatics® Data Mart. Patients with CLE or psoriasis were identified by at least two relevant International Classification of Disease-9/10 (ICD-9/10) diagnosis codes, with at least one code from a dermatologist. Patients with AD had at least one relevant ICD-9/10 code and an additional claim of asthma or allergic rhinitis. The general patient cohort was a 1% random sample of those without a diagnosis of CLE, psoriasis, or AD. The index date was the first diagnosis date for each of the CLE, psoriasis, and AD cohorts. The index date for the general patient cohort was randomly assigned to simulate the index date distribution of the other cohorts. Eligible patients were at least 18 years old on the index date. Direct costs were calculated as the sum of post-index annualized all-cause utilizations, including outpatient, medications, and hospitalization. Linear regressions with propensity score weighting assessed the cost difference across cohorts. Patient demographics were balanced across different cohorts after propensity score weighting.
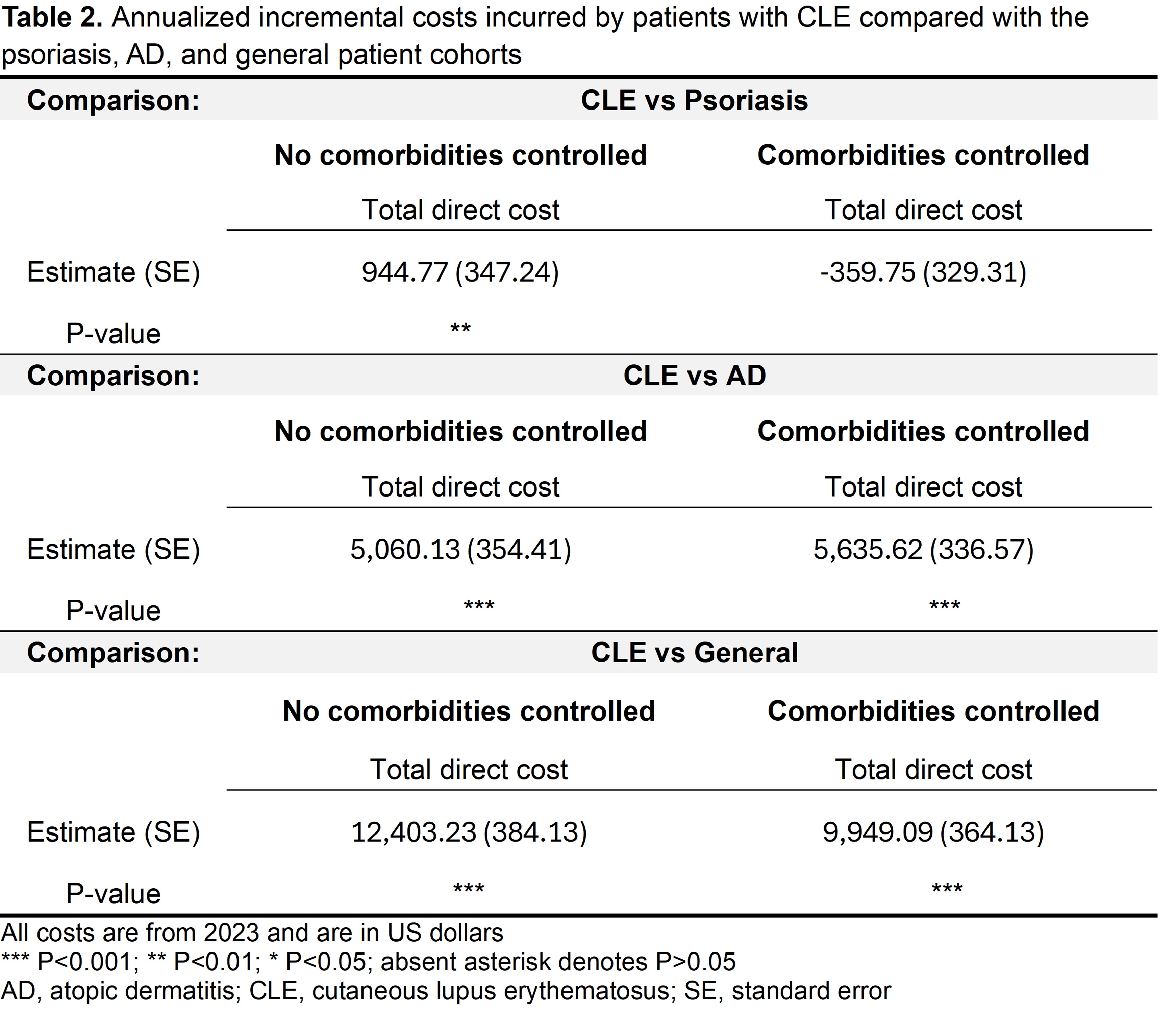
Results: The study identified 3,714 CLE, 90,133 psoriasis, 83,589 AD, and 67,221 general patients (Table 1). The CLE cohort had a higher mean age (59.5 years), and higher percentage of female (78.5%) and Black (16.2%) patients than other cohorts. In the CLE cohort, 60.0% had systemic lupus erythematosus (SLE); in the psoriasis cohort, 18.6% had psoriatic arthritis. The CLE group showed similar Charlson Comorbidity Index scores and depression and anxiety rates to the psoriasis and AD cohorts, but higher than the general population. Regression models unadjusted for comorbidities showed that patients with CLE had significantly higher total direct healthcare costs than those with AD ($5,060, P < 0.001) and the general cohort ($12,403, P < 0.001) (Table 2). The CLE annualized total cost was slightly higher than psoriasis, reaching significance ($945, P < 0.01). After comorbidity adjustment, the CLE costs remained significantly higher than the general population and AD, while the total cost difference between CLE and psoriasis became non-significant (Table 2).
Conclusion: Adults with CLE, with or without SLE, had comparable comorbidity rates to AD and psoriasis, and higher than the general population. This CLE cohort had substantially higher excess total costs than AD and the general population, and similar total cost to the psoriasis cohort. The significant healthcare costs in this population underscore health policy and societal challenges, emphasizing the need for improved management and expedited research efforts to advance therapeutic options.
To cite this abstract in AMA style:
Merola J, Mak C, Tang T, Li T, Moseley M, Gaiha-Rohrbach J, Zeng F. Direct Medical Cost Burden of Cutaneous Lupus Erythematosus (CLE): A Comparison with Psoriasis, Atopic Dermatitis, and a General Population [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/direct-medical-cost-burden-of-cutaneous-lupus-erythematosus-cle-a-comparison-with-psoriasis-atopic-dermatitis-and-a-general-population/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/direct-medical-cost-burden-of-cutaneous-lupus-erythematosus-cle-a-comparison-with-psoriasis-atopic-dermatitis-and-a-general-population/

.jpg)