Session Information
Date: Tuesday, October 28, 2025
Title: (2338–2376) Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Psoriatic arthritis (PsA) is a heterogeneous inflammatory disease with variable clinical presentation and treatment response. A subset of PsA patients are difficult to treat (D2T). This study compared baseline characteristics, extra-articular manifestations (EAMs), and comorbid conditions between D2T and non-difficult-to-treat (ND2T) PsA patients.
Methods: We performed a retrospective study using a de-identified federated database with 89 contributing healthcare organizations, including over 125 million patients (TriNetX Research Network, Cambridge, MA; date of data access: Feb 28, 2025). Patients with PsA (ICD-10: L40.59), ≥18 years, and at least one follow-up were included. We identified 7,403 adults with PsA treated with conventional DMARDs (Sulfasalazine, Methotrexate, Leflunomide) and recorded post-treatment CRP levels. There is no consensus for definition of D2T PsA, but we proposed the following: prior cDMARD use, ≥2 biologic/targeted synthetic DMARDs from two different classes and elevated CRP (≥8 mg/L). Demographics, comorbidities, and EAMs were collected. We performed 1:1 propensity score matching for age, sex, race, and ethnicity. Continuous and categorical variables were analyzed using t-tests and chi-squared tests (α = 0.05).
Results: The study included 7,403 patients (6,154 ND2T, 1,249 D2T). After propensity score matching, both groups had 1,248 patients. The D2T cohort had a higher BMI (33.1 vs. 31.7, p < 0.001) (Table 1). Comorbidities, including Crohn’s disease (3.2% vs. 1.9%, p = 0.045) and other psoriasis types (66% vs. 61.5%, p = 0.02), were more prevalent in the D2T group. D2T patients also had elevated CRP levels (50.4 vs. 28.4 mg/L, p < 0.001) and higher HLA-B27 positivity (2.2% vs. 0.8%, p = 0.005). Additionally, the D2T group demonstrated significantly greater use of biologic and targeted synthetic DMARDs across all major therapeutic classes (Table 2). TNF inhibitors were used in 88.3% of D2T patients vs. 51.9% of ND2T (p < 0.001), with adalimumab most frequently prescribed (55.2% vs. 32.8%, p < 0.001). Abatacept was also more common in D2T (15.6% vs. 1.9%, p < 0.001). IL-17 inhibitors were more frequent in D2T (86.3% vs. 15.7%, p < 0.001), primarily secukinumab (57.6% vs. 9.9%, p < 0.001). IL-23 use was higher in D2T (30.1% vs. 5.8%, p < 0.001), with guselkumab most used (18.0% vs. 3.6%, p < 0.001). IL-12/23 inhibition with ustekinumab was also more common (36.3% vs. 6.6%, p < 0.001). JAK inhibitor use was greater in D2T (31.6% vs. 5.9%, p < 0.001), mainly tofacitinib (22.7% vs. 4.1%, p < 0.001). Though rare overall, TYK2 inhibition with deucravacitinib was more common in D2T (0.8% vs. 0.2%, p = 0.021). Nearly half of the D2T group (42.4%) received four or more individual b/tsDMARDs after cDMARDs (Table 3).
Conclusion: Our study showed that in a matched cohort, D2T PsA patients had higher BMI, greater prevalence of Crohn’s disease, additional psoriasis types, higher CRP levels, and more HLA-B27 positivity. They also had significantly higher use of biologics and targeted synthetic DMARDs across all major classes.
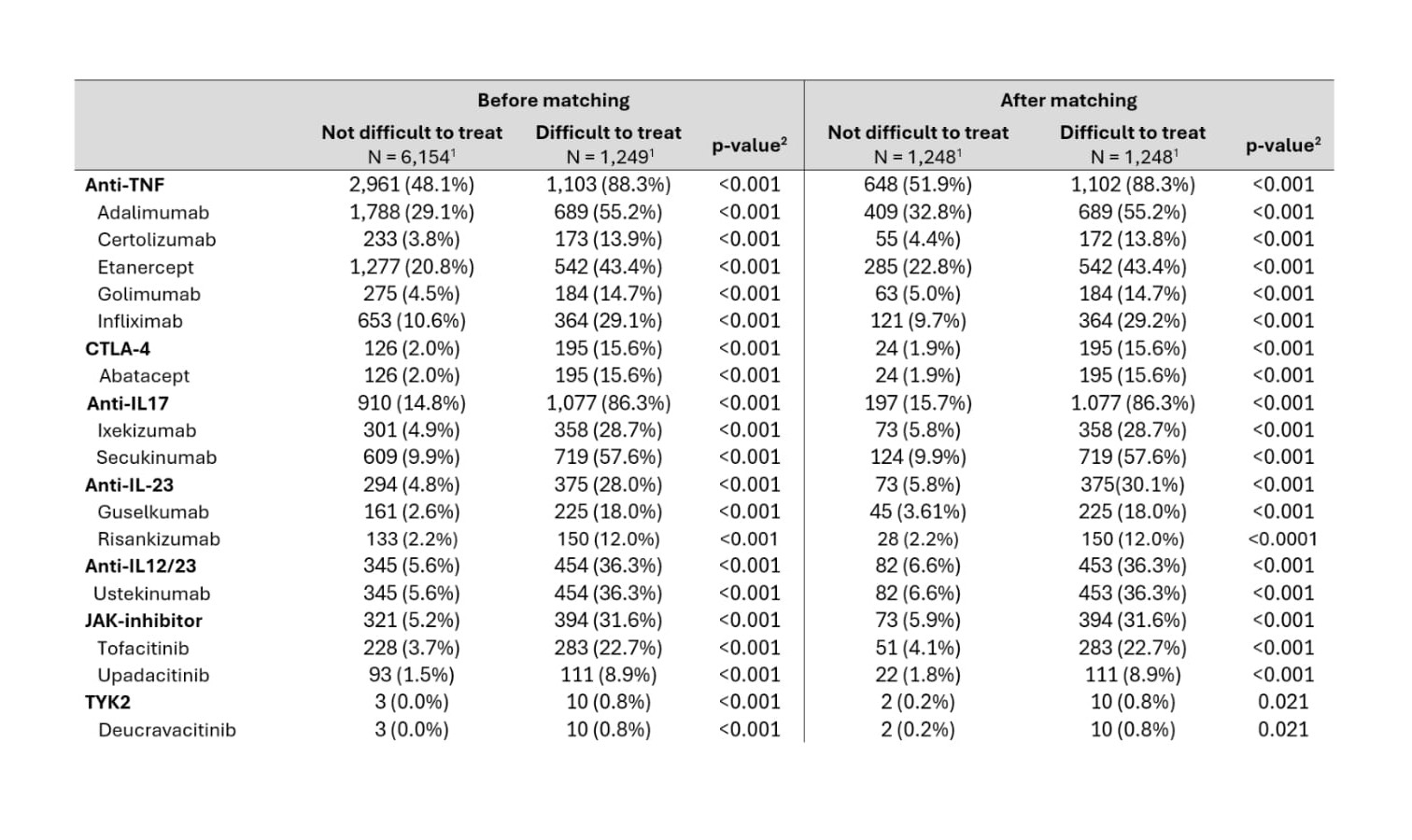 Table 1: Baseline characteristics between difficult to treat and not difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
Table 1: Baseline characteristics between difficult to treat and not difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
.jpg) Table 2: Use of biologic and targeted synthetic DMARDs between not difficult to treat and difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
Table 2: Use of biologic and targeted synthetic DMARDs between not difficult to treat and difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
.jpg) Table 3: Number of drug classes and total biologic and targeted synthetic used between difficult to treat and not difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
Table 3: Number of drug classes and total biologic and targeted synthetic used between difficult to treat and not difficult to treat psoriatic arthritis, before and after propensity score matching for demographics (age, sex, race, and ethnicity).
To cite this abstract in AMA style:
Heydari-Kamjani M, Murphy J, Magrey M. Real-World Characteristics and Treatment Patterns of Difficult-to-Treat Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/real-world-characteristics-and-treatment-patterns-of-difficult-to-treat-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-world-characteristics-and-treatment-patterns-of-difficult-to-treat-psoriatic-arthritis/
