Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Targeted synthetic and biologic DMARDs have transformed psoriatic arthritis (PsA) treatment. Still, a substantial subset of patients reports persistent joint pain despite well-controlled inflammation. We previously demonstrated that such patients fare worse across multiple PSAID domains. In this study, we aimed to more precisely characterize the psychological and functional profile of this potentially distinct phenotype.
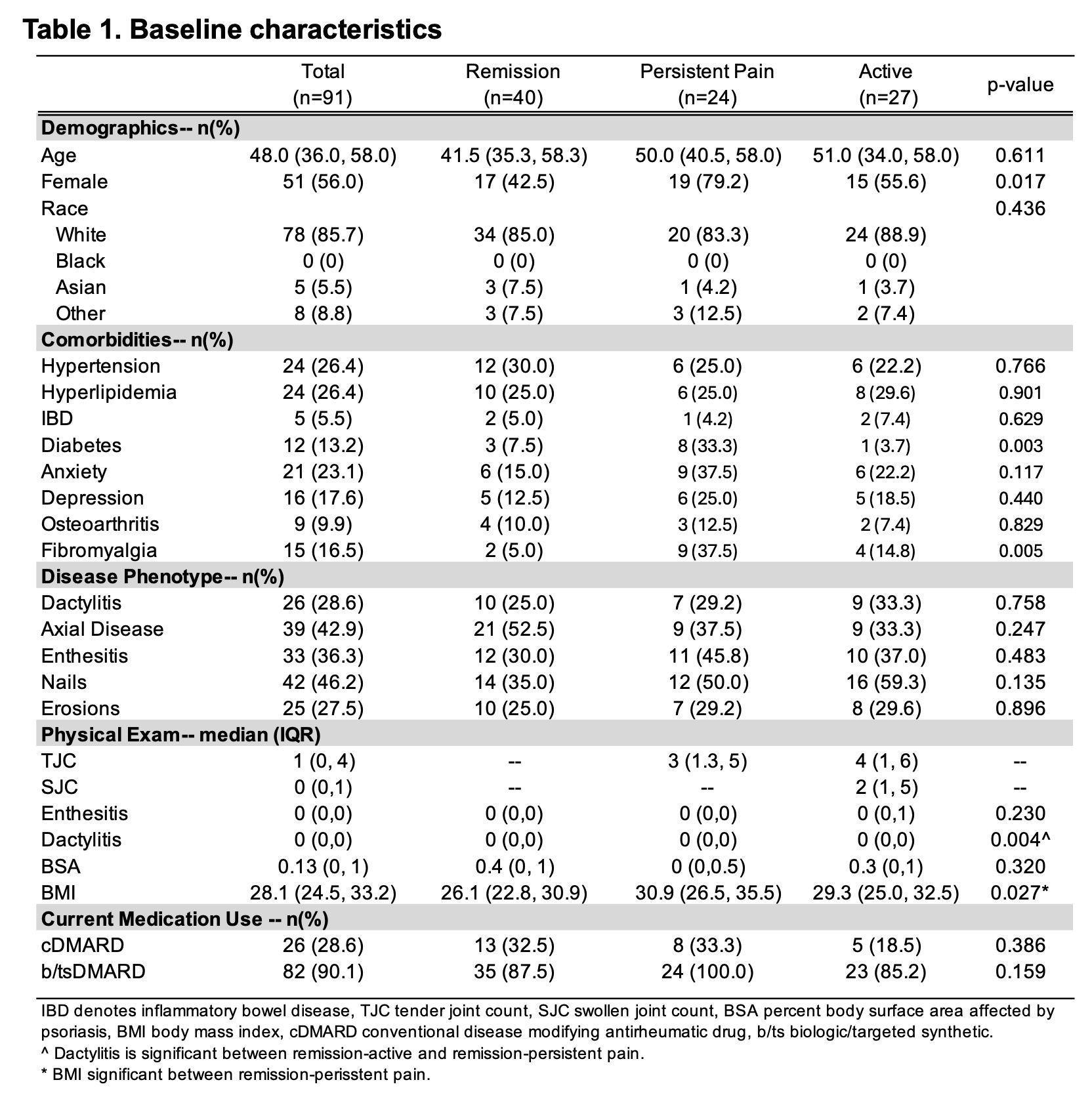
Methods: PsA patients meeting CASPAR criteria were prospectively enrolled at the NYU Psoriatic Arthritis Center. Participants underwent a standardized clinical evaluation and completed multiple surveys, including Pain Catastrophizing Scale (PCS), Functional Assessment of Chronic Illness Therapy-Fatigue Scale (FACIT-F), Hospital Anxiety and Depression Scale (HADS- A/D), Patient Health Questionnaire-9 (PHQ-9), RAPID3, PROMIS29, and EQ-5D. Patients were categorized into three groups: active (≥1 SJC, ≥0 TJC), persistent pain (0 SJC, ≥1 TJC), or remission (0 SJC, 0 TJC). Summary data was presented as numbers/percentages or medians/interquartile regions (IQR). Group comparisons were performed using Chi-squared tests and Kruskal-Wallis tests with post-Hoc Dunn’s test for pair-wise comparisons with Bonferroni correction.
Results: 91 patients were assessed; 24 (26.4%) had persistent joint pain, 40 (43.9%) were in remission, and 27 (29.7%) had active inflammation (Table 1). Patients with persistent pain were more likely to be female (p=0.02), meet criteria for fibromyalgia (p=0.005), and have diabetes (p=0.003). Compared to those in remission, patients with persistent pain had a higher body mass index (30.9 (IQR 26.5, 35.5) vs 26.1 (22.8, 30.9), p=0.022) and worse psychologic profiles (Figure 2). They demonstrated higher levels of catastrophizing (PCS 11 ( 5.0, 15.8) vs 1.5 (0, 10.0), p= 0.004), depressive symptoms (PHQ-9 6.0 (48.6, 62.1) vs 2.5 (0.3, 4), p=0.001; HADS-D (5.0 (3.0, 8.5) vs 2.0 (0, 5.0), p=0.011) and fatigue (FACIT 33.0 (20.8, 42.8) vs 44.0 (40.0, 47.5), p < 0.001). There was no difference in anxiety level (HADS-A 6.5 (4.0, 11.8) vs 5.0 (2.0, 6.0), p=0.256). They reported decreased physical function (41.6 (37.0, 45.0) vs 47.6 (42.1, 56.9), p < 0.001), decreased ability to participate in social activities (48.2 (39.0, 51.8) vs 57.6 (48.2, 64.2), p= 0.004), more pain interference, (56.7 (52.2, 62.1) vs 51.7 (41.6, 55.7), p=0.008) and worse overall QoL (EQ5D 0.63 (0.4, 0.8) vs 0.8 (0.7, 0.9), p < 0.001 ). Patients with persistent pain had profiles similar to those with active inflammatory disease (and in many domains were numerically worse, Table 2).
Conclusion: Persistent joint pain in PsA, even without objective inflammation, is linked to a reproducible cluster of psychosocial distress and functional impairment. These patients may not fit the traditional treat-to-target approaches that focus on inflammation mitigation alone. Our findings underscore an unmet therapeutic need: integrative interventions targeting depression, fatigue, and catastrophizing—such as cognitive behavioral therapy or pharmacologic treatment of mood disorders— which may be critical to achieving remission and improving quality of life in PsA.
To cite this abstract in AMA style:
Haberman R, Chen K, Felipe A, Eichman S, Scher U, Scher J. Persistent Pain in PsA: A Distinct Phenotype of Depression, Fatigue, And Catastrophizing [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/persistent-pain-in-psa-a-distinct-phenotype-of-depression-fatigue-and-catastrophizing/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistent-pain-in-psa-a-distinct-phenotype-of-depression-fatigue-and-catastrophizing/

.jpg)
.jpg)