Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Inflammatory bowel disease (IBD)-associated arthritis (IBD-A) can affect 24-44% of IBD patients and may represent an enhanced inflammatory state. IBD-A patients often experience a more severe disease course, increased hospitalizations, a higher need for surgical or biologic therapies, and worse outcomes compared to IBD alone. Prior studies have examined the reasons for hospitalizations for IBD, but the inpatient burden of IBD-A remains underexplored. Understanding differences in sociodemographic characteristics and healthcare utilization in patients with IBD-A vs IBD alone may help inform resource management and policy
Methods: We used the National Inpatient Sample (NIS) database to identify adult hospitalizations with a primary or secondary diagnosis of IBD from 2016 to 2020. Admissions with concurrent diagnosis of IBD-A were identified using ICD-10 codes. We compared demographics, insurance type, median household income, geographic location, length of stay (LOS), total hospital charges, and in-hospital mortality between patients with IBD-A and IBD alone. Survey-weighted analyses were used to generate national estimates. A p-value < 0.05 was considered statistically significant.
Results: A total of 1880 adult IBD-A hospitalization events were included. The top reasons for hospitalizations for IBD-A patients were: Ulcerative colitis (12.2%), followed by sepsis (10.6%), and then Crohn’s disease with and without complications (6.0%). Compared with IBD patients without arthritis, patients with IBD-A were more likely to be younger (median age 42 vs 55 years, p value < 0.001) and females (64.1% versus 56.2%, p value 0.002), more frequently had private insurance (48.1% vs 35.9%, p value < 0.001) or Medicaid (21.3% vs 14.7%, p value < 0.001), and less commonly were from lowest quartile of household income [$1 - 55,999] (16.2 % vs 24.1%, p value < 0.001). Geographically, compared to IBD-only patients, IBD-A admissions were more common in the Northeast (28.5% vs 21.5%, p value 0.002) and West (21.7% vs 17.1%, p value 0.046) and less frequent in the South (22.3% vs 36.7%, p value < 0.001). Compared to IBD admissions, IBD-associated arthritis admissions had a similar length of stay, total hospital charges, and in-hospital mortality (1.1% vs 1.6%) as shown in Table 1.
Conclusion: Hospitalizations with IBD-A were more prevalent in younger people and females. There were no differences in race/ethnicity, length of stay, or total hospital charges between the two groups of patients. Future studies should investigate the causes of admissions in patients who are younger and female, and explore if they are sub-optimally treated for their IBD or arthritis, leading to more hospitalizations.
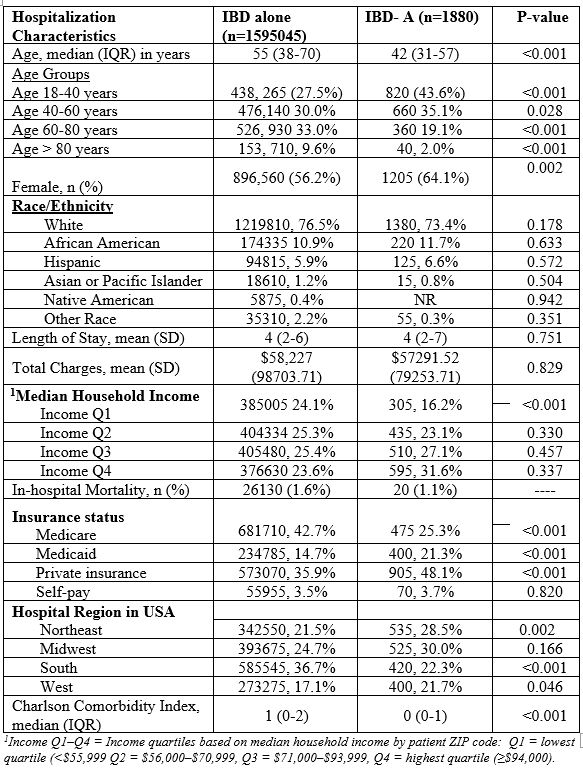 Table 1. Weighted Descriptive Characteristics of IBD-associated Arthritis (IBD-A) Hospitalizations from the 2016-2020 National Inpatient Sample (n=1880)
Table 1. Weighted Descriptive Characteristics of IBD-associated Arthritis (IBD-A) Hospitalizations from the 2016-2020 National Inpatient Sample (n=1880)
To cite this abstract in AMA style:
Sami F, Danila M, Caplan L, Sen R. Sociodemographic Characteristics and Healthcare Utilization in Patients with IBD-Associated Arthritis vs. IBD Alone: A Nationwide Inpatient Analysis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/sociodemographic-characteristics-and-healthcare-utilization-in-patients-with-ibd-associated-arthritis-vs-ibd-alone-a-nationwide-inpatient-analysis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/sociodemographic-characteristics-and-healthcare-utilization-in-patients-with-ibd-associated-arthritis-vs-ibd-alone-a-nationwide-inpatient-analysis/
