Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with psoriasis and psoriatic arthritis (PsA) are at increased risk for metabolic comorbidities and poorer long-term outcomes compared to the general population. Identifying patients at risk for adverse outcomes can facilitate targeted interventions to improve quality of life.This study aimed to evaluate the risk of hospitalization and emergency department (ED) visits among adults with psoriatic disease and identify predictors of these outcomes.
Methods: We utilized data from the Forward Psoriasis Registry, a cohort recruited from U.S. dermatology practices, two academic institutions, and the Forward registry website. Participants enrolled between August 2023 and March 2025 completed baseline and monthly surveys, with longer assessments every six months. Surveys included comorbidity data, psoriasis severity (measured by the Patient Report of Extent of Psoriasis Involvement [PREPI]), patient-reported outcomes (Psoriasis Symptoms and Signs Diary [PSSD]), medication changes, and adverse events, including hospitalization and ED visits. Participants with psoriasis (with or without PsA) who completed enrollment and had at least one follow-up visit were included. We report baseline demographics, disease characteristics, treatments, and comorbidities. Cox proportional hazards models were used to identify predictors of hospitalization and ED visits, with a multivariable model developed using purposeful selection modeling.
Results: ong 2,606 enrollees, 1,354 had at least one follow-up visit, with a mean follow-up time of 213 days (SD 145). The cohort had a mean age of 51 years (SD 16), 66% were female, and 56% were from the southern United States. Most had mild to moderate psoriasis (23% with < 1% BSA, 40% with 1-2% BSA, 30% with 3-10% BSA, and 6% with >10% BSA). A total of 135 participants experienced an ED visit (incidence 0.18 per person-year), and 59 were hospitalized (incidence 0.08 per person-year). Predictors of ED visits and hospitalization were similar. Lower psoriasis severity (< 1% BSA) was associated with the lowest risk for both outcomes. Higher PSSD scores, depression, and female sex were significantly associated with increased risk. Although a diagnosis of ADHD was initially significant, it was removed from the final model due to lack of consistency.
Conclusion: In this cohort with psoriatic disease, predictors of hospitalization and ED visits included higher PSSD scores, depression, and female sex. The PSSD, a patient-reported outcome, demonstrated predictive value beyond the psoriasis severity measured by body surface area, underscoring the importance of patient-reported outcomes in assessing disease impact.
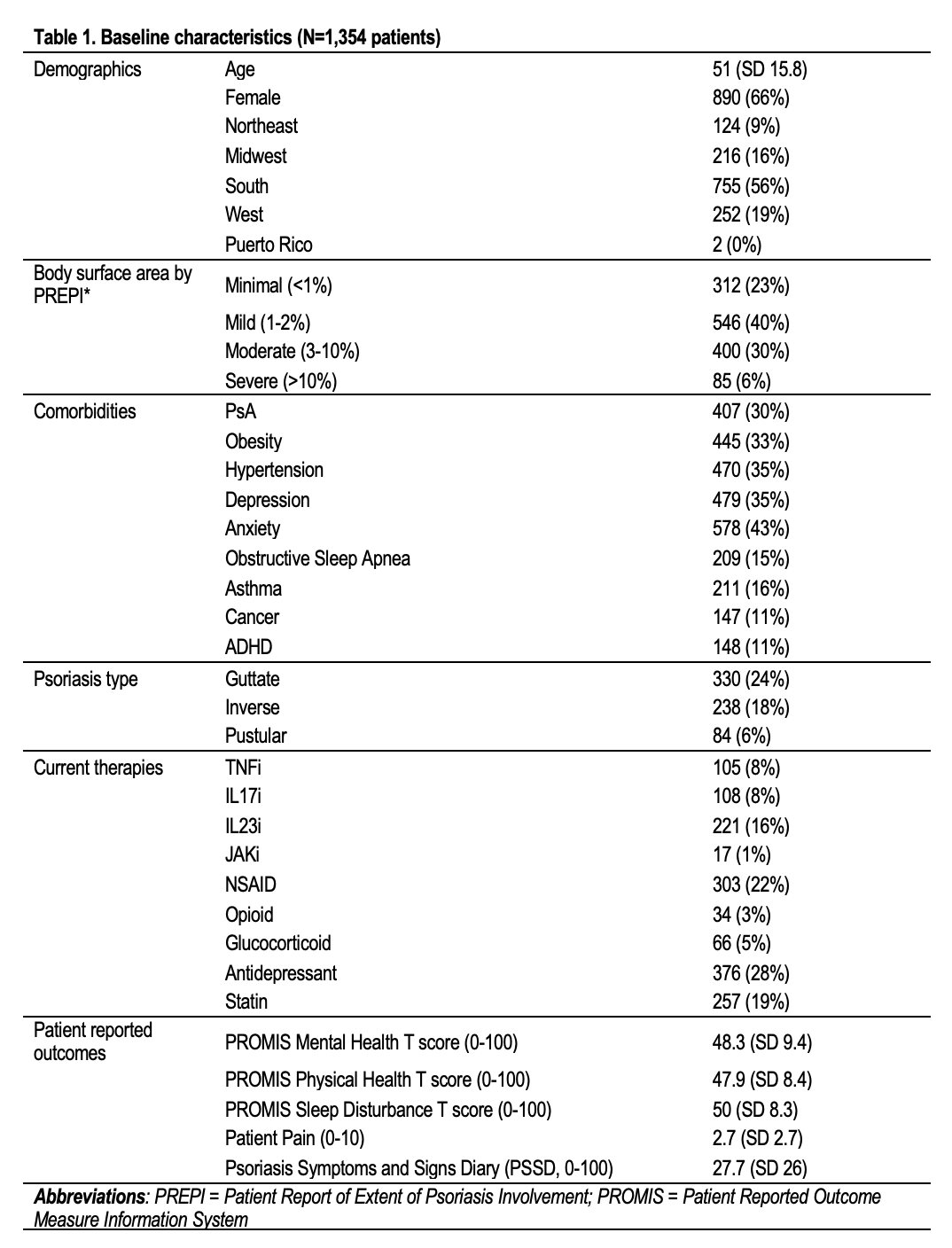 Table 1. Baseline Characteristics
Table 1. Baseline Characteristics
.jpg) Table 2. Univariable and multivariable models
Table 2. Univariable and multivariable models
To cite this abstract in AMA style:
Ogdie A, Romich E, Coburn B, Schumacher R, Michaud K. Predictors of Hospitalization and Emergency Department Visits Among Patients with Psoriatic Disease: Insights from the Forward Psoriasis Registry [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/predictors-of-hospitalization-and-emergency-department-visits-among-patients-with-psoriatic-disease-insights-from-the-forward-psoriasis-registry/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/predictors-of-hospitalization-and-emergency-department-visits-among-patients-with-psoriatic-disease-insights-from-the-forward-psoriasis-registry/
