Session Information
Date: Tuesday, October 28, 2025
Title: (2195–2226) Reproductive Issues in Rheumatic Disorders Posters
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Despite significant advances in SLE management, women with systemic lupus erythematosus (SLE) are at risk of adverse pregnancy outcomes (APOs). We sought to determine the risk and risk factors for maternal APOs among females with SLE in the US.
Methods: Using a large, multicenter, electronic health record (EHR) database (TriNetX), we performed a retrospective cohort study of reproductive-age females (age 15-44 years) with SLE. SLE was defined by ≥2 ICD codes >30 days and < 2 years apart. We identified pregnancies occurring before and after SLE diagnosis using ICD and CPT codes. We assessed APOs identified by ICD codes, including pre-eclampsia, preterm delivery, peripartum infection, venous thromboembolism, cardiomyopathy, maternal death, and a composite outcome including any of these events. We also assessed postpartum hospitalizations for SLE. We assessed potential risk factors, including demographics, geographic region, SLE severity index, SLE manifestations of lupus nephritis (LN) and antiphospholipid antibody syndrome (APS), and medication use in the six months prior to pregnancy onset, including hydroxychloroquine, oral glucocorticoids, belimumab, and known teratogenic immunosuppressant medications (i.e., methotrexate, mycophenolate, or leflunomide). We used multivariate logistic regression analysis to compare the odds of APOs according to potential risk factors.
Results: From January 2000 to August 2021, we identified 41,558 females of childbearing age with SLE and 9,180 with ≥1 pregnancy before or after the first SLE code (Table 1). There were 12,598 total SLE pregnancies, with 7,539 occurring before and 5,059 occurring after SLE diagnosis. Among pregnancies that occurred after diagnosis, 15.7% were exposed to teratogens within 6 months prior to pregnancy. The incidence of composite APOs among total SLE pregnancies was 22.8% (Table 2). Pre-eclampsia (11.4%), hospitalization for SLE (8.5%), and thromboembolism (8.0%) were the most common adverse maternal outcomes. Black and Hispanic patients were at increased risk for composite APOs and SLE hospitalizations (aORs for composite APOs: 1.34 [95% CI 1.17-1.53] and 1.20 [1.03-1.41]) for Black and Hispanic patients compared to White patients, respectively, and aORs for SLE hospitalizations: 1.42 [1.19-1.69] and 1.32 [1.07-1.62] for Black and Hispanic patients compared to White patients, respectively). Patients with severe disease were at 3 times higher odds of APOs (Table 3) and a higher risk of SLE hospitalization (aOR 1.73, CI 95% 1.37-2.20). APS and LN also increased the risk of APOs and hospitalizations. When adjusted for SLE severity, medication use was not associated with the risk of composite APOs.
Conclusion: In this large EHR-based cohort of SLE pregnancies, we identified a high burden of composite and specific APOs. Patient factors associated with higher risks of APOs included Black race, Hispanic ethnicity, higher SLE severity, and disease manifestations of LN and APS. These findings highlight the importance of pregnancy counseling for reproductive-age females with SLE and efforts to improve maternal pregnancy care and outcomes.
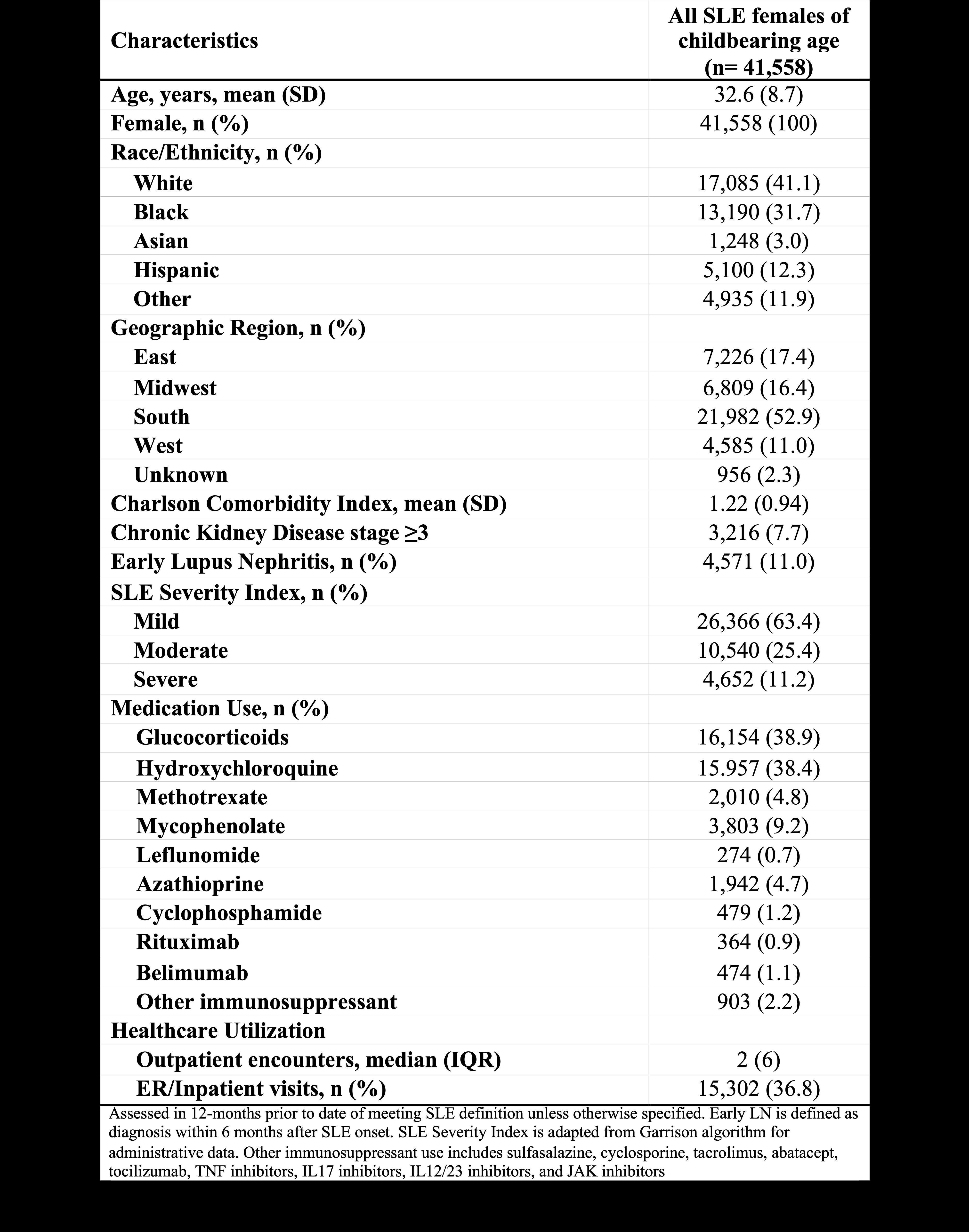 Table 1. Characteristics of Females of Reproductive Age with SLE
Table 1. Characteristics of Females of Reproductive Age with SLE
.jpg) Table 2. Maternal Adverse Pregnancy Outcomes in Patients with Systemic Lupus Erythematosus
Table 2. Maternal Adverse Pregnancy Outcomes in Patients with Systemic Lupus Erythematosus
.jpg) Table 3. Risk Factors for Composite Adverse Pregnancy Outcomes
Table 3. Risk Factors for Composite Adverse Pregnancy Outcomes
To cite this abstract in AMA style:
Lee G, Nestor J, Zhou B, Jorge A. Maternal Adverse Pregnancy Outcomes and Risk Factors in Patients with Systemic Lupus Erythematosus in the United States [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/maternal-adverse-pregnancy-outcomes-and-risk-factors-in-patients-with-systemic-lupus-erythematosus-in-the-united-states/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/maternal-adverse-pregnancy-outcomes-and-risk-factors-in-patients-with-systemic-lupus-erythematosus-in-the-united-states/
