Session Information
Date: Tuesday, October 28, 2025
Title: (1972–1989) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Influenza and pneumococcal infection can cause mild to severe illness and potentially lead to serious complications or death. Patients with rheumatic diseases have weakened immune defenses due to the disease and immunosuppressive therapy, increasing their risk of infections and complications. The American College of Rheumatology recommends the high-dose or adjuvanted influenza vaccine and the pneumococcal vaccine for patients with rheumatic or musculoskeletal diseases on immunosuppressive therapy. Despite these guidelines, vaccination rates in this population remains suboptimal. Barriers include lack of provider prompts, inconsistent vaccination documentation, and lack of or vaccine misinformation for patients. Our goal is to improve vaccination rates in Rheumatology clinic to protect this vulnerable population.
Methods: Baseline data on influenza and pneumococcal vaccination rates were collected from November 1, 2023 to March 31, 2024 (Period 1). During each visit, patients received a questionnaire to assess vaccine status and interest. Providers and clinic staff attended an educational session outlining the importance of vaccination in immunosuppressed patients, project objectives, and strategies for identifying eligible patients using the questionnaire and electronic medical record care gap alerts. Post-intervention vaccination rates were assessed from November 1, 2024, to March 31, 2025 (Period 2).
Results: Baseline data collected from period 1 revealed administration of 69 influenza vaccines and 2 Pneumococcal (Prevnar 20) vaccines. Following implementation of our intervention, period 2 data demonstrated a marked rise in vaccination rates, with 144 influenza vaccines administered – an 108.9% increase – and 170 Prevnar 20 vaccines administered, reflecting an 8,400% increase. The mean number of influenza vaccines each month was 13.8 and 29.6 in period 1 and 2 respectively with a p-value of 0.144. The mean number of pneumococcal vaccines each month was 0.4 and 34.6 in period 1 and 2 respectively with a p-value of 0.010.
Conclusion: Vaccinations are crucial in patients with rheumatic and musculoskeletal diseases and receiving immunosuppressive therapy. Baseline data revealed low influenza and pneumococcal vaccine rates, highlighting a critical gap in preventative care. After implementing patient questionnaires and staff education, we observed a marked increase in vaccine uptake—suggesting that targeted interventions with a multidisciplinary team of physicians and ancillary medical staff can effectively improve vaccination rates in high-risk populations. Challenges included inconsistent use of the questionnaire after a few months which was partially mitigated through staff reminders. Furthermore, an area for improvement was ensuring patients receive the high-dose or adjuvanted influenza vaccine when indicated. Limitations included inconsistent access to up-to-date vaccination records and therefore not having denominators for statistical analysis. Moving forward, ongoing education, tracking, and extended outreach are necessary to sustain improvements, ensure administration of indicated vaccines, and further reduce the risk of preventable infections.
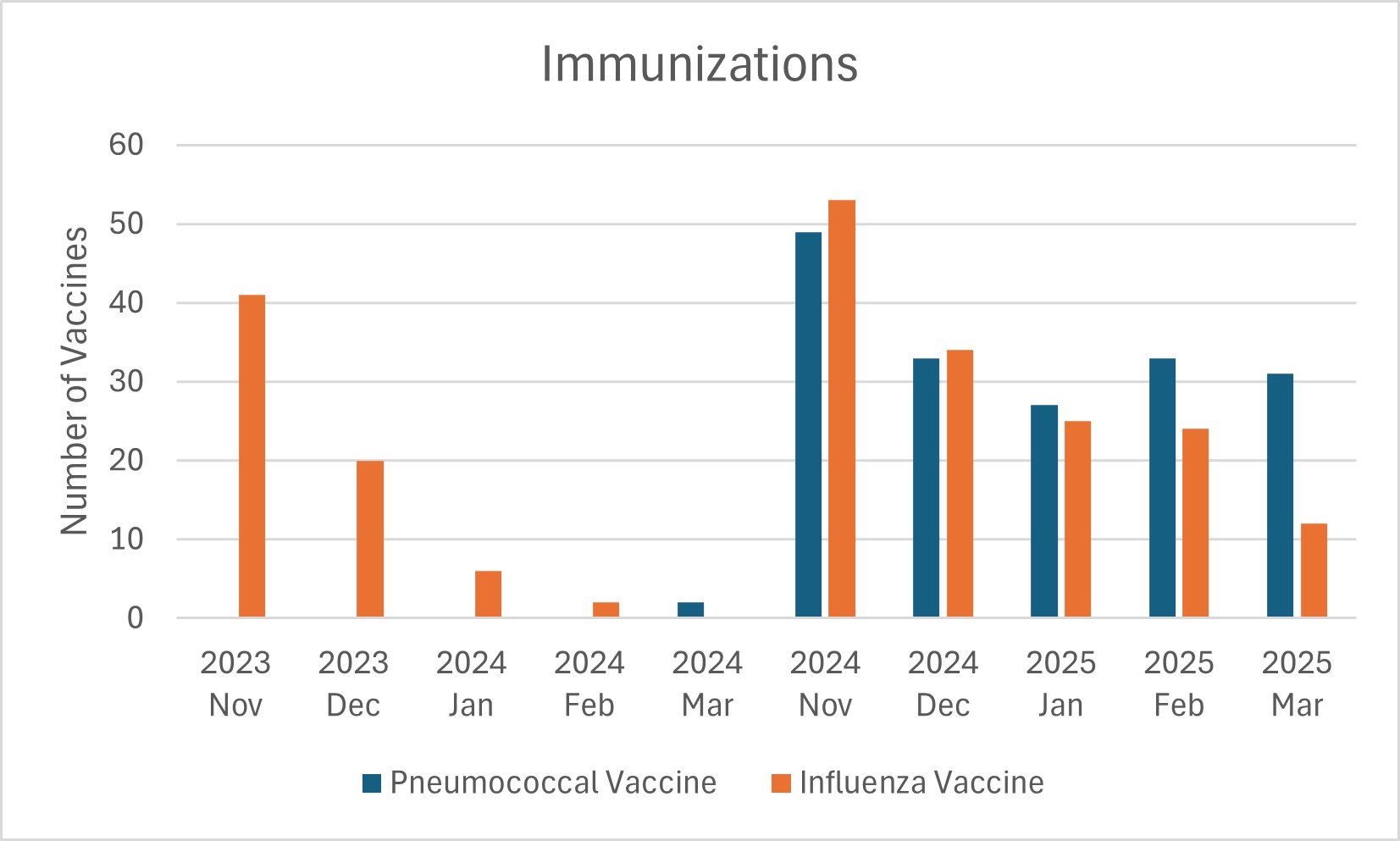 Pneumococcal and Influenza Vaccination Rates from November 1, 2023 to March 31, 2024 and from November 1, 2024 to March 31, 2024.
Pneumococcal and Influenza Vaccination Rates from November 1, 2023 to March 31, 2024 and from November 1, 2024 to March 31, 2024.
To cite this abstract in AMA style:
Patel K, Paudyal S, Hurley D. Improving Vaccination Rates in the Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/improving-vaccination-rates-in-the-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-vaccination-rates-in-the-rheumatology-clinic/
