Session Information
Date: Monday, October 27, 2025
Title: (1612–1632) Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: European Alliance of Associations for Rheumatology (EULAR) recommendations for the management of Polymyalgia Rheumatica (PMR) and Large Vessel Vasculitis (LVV) date back to 2015 and 2020 respectively. Novel evidence about their management has emerged since then.This study aims to systematically review the recent literature on the referral and diagnosis of PMR and LVV to inform the related EULAR recommendations.
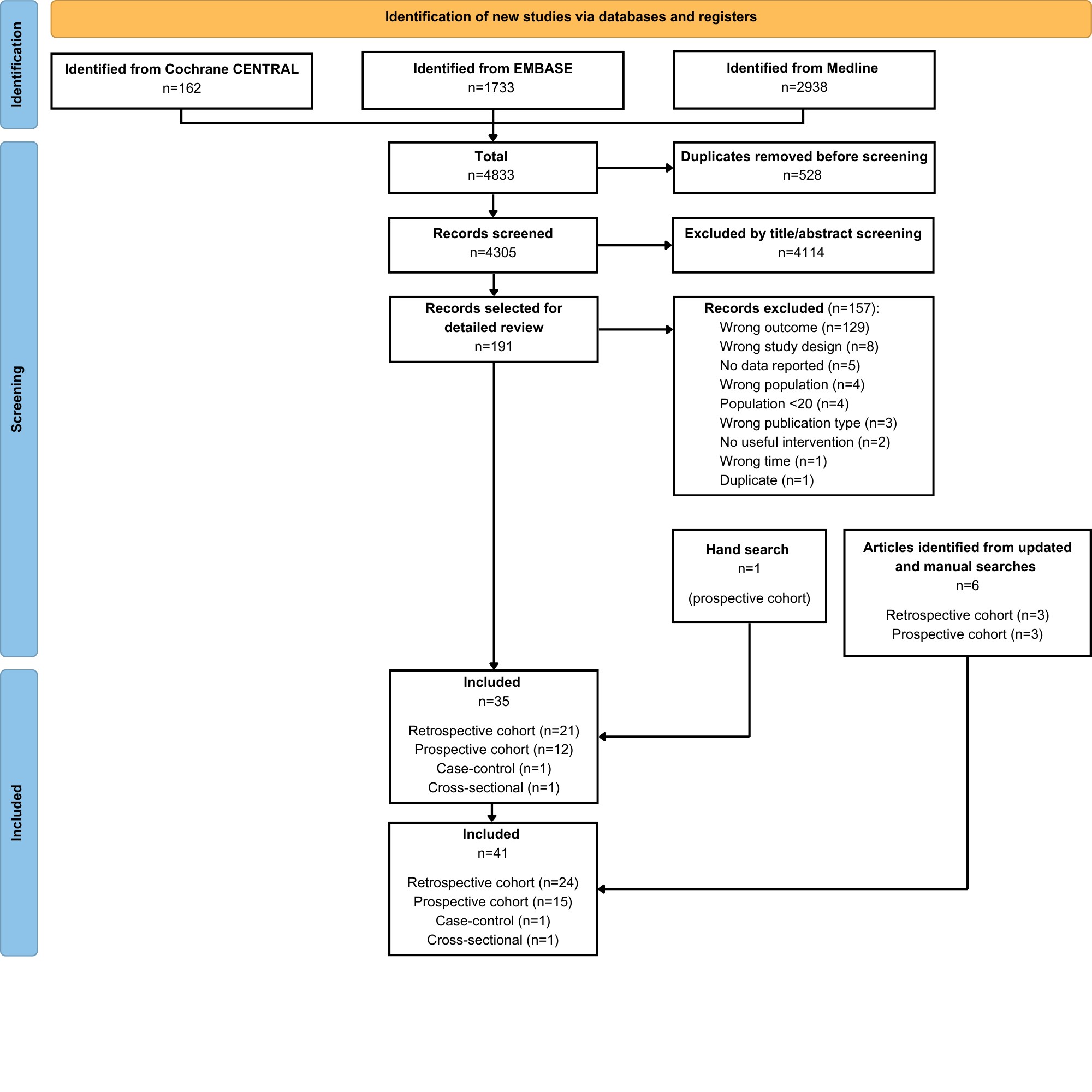
Methods: A systematic review (PROSPERO CRD42024560403) focused on PMR, giant cell arteritis (GCA) and Takayasu arteritis (TAK) referral and diagnosis, was conducted across MEDLINE, Embase, and Cochrane databases with publications dating from May 2014 for PMR, and January 2018 for LVV, up to December 2024. No language restriction was applied. Age was limited to adults above 18 years. Randomised trials, observational studies (cohort, case-control, cross-sectional), systematic reviews and meta-analyses were included. Studies of single imaging modalities were outside the remit of the project. EULAR 2024 and American College of Rheumatology 2024 congress abstracts were additionally screened to identify relevant studies published after the end date of the search. Relevant risk of bias tools were used to assess study quality.
Results: Forty-one studies (all observational) met the inclusion criteria (Figure 1).Fast-track clinics (FTC) for suspected GCA (3 studies, n=682) reduced the risk of blindness from 19–27% to 12–13% and shortened the time to diagnosis from a median of 62 days to 33 days (p=0.04). FTC for suspected PMR (3 studies, n=662) reduced the diagnostic latency (7–53 days FTC vs 12–80 days controls, p=0.001) and the hospitalisation rate (3.5% FTC vs 20.4% controls, p=0.001).Ten studies investigating the presence of subclinical LVV in patients with a PMR-like presentation have been retrieved (n=1229). The clinical presentation of isolated PMR and subclinical LVV was similar. However, subclinical LVV had a higher risk of relapse and greater need for immunosuppression (Table 1).Ten studies (n=1047) confirmed similar or superior performance of imaging, namely temporal and axillary artery ultrasound (US) or positron emission tomography (PET) compared to temporal artery biopsy (TAB) alone for the diagnosis of GCA in terms of sensitivity and rapidity of diagnosis. Moreover, multimodal diagnostic pathways (9 studies, n=2470) integrating pre-test probability scores, imaging and/or TAB increased the accuracy of GCA diagnosis. A pathway based on US, followed by PET, and ultimately an expert clinician’s opinion was more sensitive than TAB (92% vs 39%) and decreased the diagnostic delay (1.1 days US, 1.9 days PET, 10.8 days TAB). Glucocorticoids (GC) rapidly reduced the sensitivity of TAB (5 studies): 23–74% GC < 1 week vs 20–52% GC > 1 week – OR 0.36, 95% CI 0.13–0.96 (p=0.04).No new high-quality evidence emerged concerning the referral and diagnosis of TAK.
Conclusion: This systematic review provides new insights into the referral and diagnosis of PMR and LVV, including the value of multimodal FTC pathways, the use of US in the workup of PMR and LVV, and subclinical LVV in patients presenting with PMR-like symptoms. This evidence will inform the 2025 EULAR recommendations for the management of PMR and LVV.
.jpg) Table 1. Outcomes of subclinical LVV vs isolated PMR. DMARD disease-modifying antirheumatic drug, GC glucocorticoid, LVV large vessel vasculitis; MPDN, methylprednisolone; PDN, prednisone; PMR polymyalgia rheumatica.
Table 1. Outcomes of subclinical LVV vs isolated PMR. DMARD disease-modifying antirheumatic drug, GC glucocorticoid, LVV large vessel vasculitis; MPDN, methylprednisolone; PDN, prednisone; PMR polymyalgia rheumatica.
To cite this abstract in AMA style:
Bartoletti A, Ducker G, Dey M, Misra D, Monti S, Hellmich B, Mukhtyar C, Studenic P, Nikiphorou E. A Systematic Literature Review to Inform the EULAR Recommendations for the Management of Polymyalgia Rheumatica and Large Vessel Vasculitis: Focus on Referral and Diagnosis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/a-systematic-literature-review-to-inform-the-eular-recommendations-for-the-management-of-polymyalgia-rheumatica-and-large-vessel-vasculitis-focus-on-referral-and-diagnosis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a-systematic-literature-review-to-inform-the-eular-recommendations-for-the-management-of-polymyalgia-rheumatica-and-large-vessel-vasculitis-focus-on-referral-and-diagnosis/