Session Information
Date: Monday, October 27, 2025
Title: (1221–1247) Pain in Rheumatic Disease Including Fibromyalgia Poster
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Fibromyalgia (FM) is a stress-related disorder in which dorsal root ganglia (DRG) may play a pivotal pathogenetic role. DRG exhibit unique stress-induced, pro-algesic physio-anatomy, where each pain-sensing nerve fiber soma is tightly encased by metabolically active, immune-competent satellite glial cells (SGCs). Mice receiving IgG from patients with FM display mechanical and cold hypersensitivity and small nerve fiber pathology, in these instances patients IgG is exclusively deposited in mouse DRG SGCs. A subgroup of patients suffering from severe FM harbors anti-SGCs antibodies, although the specific antibody target(s) remain unidentified.Glial fibrillary acidic protein (GFAP) is an intermediate filament protein serving as an early SGCs activation marker. Different environmental stressors induce GFAP cell-surface expression that could conceivably serve as novel antigen. GFAP antibodies have been implicated in autoimmune encephalomyelitis.This proof-of-concept study aimed to determine whether the serum of patients suffering from FM contains antibodies against GFAP.
Methods: We included 47 women with “primary” FM (meeting ACR 2010 and Wolfe et al 2016 criteria) without concurrent autoimmune rheumatic disease and 31 age-, sex-, and BMI-matched healthy controls. All participants completed the following standardized clinimetric questionnaires: 2016 Wolfe et al criteria, FIQ-R, COMPASS-31, Small Fiber Symptom Survey, S-LANSS, PHQ-9, GAD-7, IPAQ, and EuroQol-5D. A sensitive ELISA was developed using recombinant human GFAP (Abcam, Waltham, MA, USA) coated on 96-well plates. Serum samples were incubated overnight, followed by detection with HRP-conjugated anti-human IgG. Each plate included a positive control (commercial anti-GFAP antibody).
Results: Patients with FM exhibited higher GFAP antibody optical densities (OD) compared to controls (median 0.04, 0.02–0.10 vs. 0.02, 0.01–0.05; p = 0.025). Using the controls 99th percentile value (0.127 OD) as cut-off point, 9/47 (19%) of patients suffering from FM tested positive for anti-GFAP antibodies (figure 1). This antibody positivity ratio yields a sensitivity of 19%, specificity of 97%, positive predictive value of 90%, and negative predictive value of 44%. No significant differences in clinimetric scores were observed between GFAP-positive versus GFAP-negative patients.
Conclusion: A subset of patients suffering from FM harbors serum antibodies against GFAP. Whether these antibodies are more prevalent in cerebrospinal fluid of individuals with FM, as seen in GFAP-associated autoimmune encephalomyelitis, remains to be determined. These early findings suggest that abnormal GFAP expression may play a role in the pathogenesis of FM, warranting further investigation of FM as satellite gliopathy.
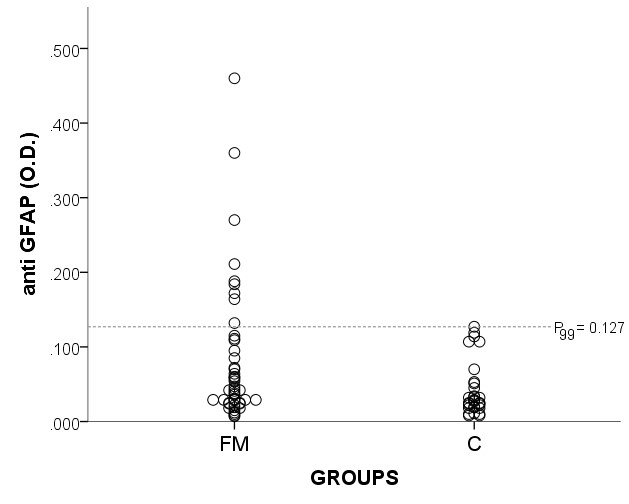 ELISA detection of GFAP antibodies in patients suffering from fibromyalgia (FM) and controls (C) using the controls 99th percentile as threshold for antibody positivity.
ELISA detection of GFAP antibodies in patients suffering from fibromyalgia (FM) and controls (C) using the controls 99th percentile as threshold for antibody positivity.
To cite this abstract in AMA style:
Massó F, Martinez-Martinez L, Amezcua-Guerra L, Mercado F, Almanza A, Martínez-Lavín M. Serum Antibodies Against Glial Fibrillary Acidic Protein in Fibromyalgia: A Proof-of-Concept Study [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/serum-antibodies-against-glial-fibrillary-acidic-protein-in-fibromyalgia-a-proof-of-concept-study/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/serum-antibodies-against-glial-fibrillary-acidic-protein-in-fibromyalgia-a-proof-of-concept-study/
