Session Information
Date: Monday, October 27, 2025
Title: (1147–1190) Miscellaneous Rheumatic & Inflammatory Diseases Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Haploinsufficiency of A20 (HA20) is a disease at the crossroads between autoinflammation and autoimmunity, caused by heterozygous mutations in TNFAIP3, which encodes the A20 protein, a negative regulator of proinflammatory pathways such as NF-κB and NLRP3. Clinically, HA20 can mimic systemic lupus erythematosus, Behçet’s disease, inflammatory bowel disease, familial Mediterranean fever, or PFAPA syndrome. Hallmark features include recurrent fever, bipolar aphthosis, skin and gastrointestinal inflammation. Genetic testing is required for diagnosis. Our study aimed to assess the prevalence of relevant mutations in a cohort with clinically suggestive features, to improve diagnostic precision in daily rheumatology practice.
Methods: Fourteen patients were prospectively recruited from the Rheumatology Department at University Hospital Puerta de Hierro, meeting inclusion criteria based on current literature. Recurrent oral aphthosis before age 30 was required, along with one or more of the following: unexplained fever, genital aphthosis, arthritis/arthralgia, acneiform/pustular/erythema nodosum-like skin lesions, recurrent abdominal pain or diarrhea, or inflammatory ocular disease. Data collected included demographics, family history, age at symptom onset, mucosal, cutaneous, articular, gastrointestinal, and ocular involvement, and fever episodes. Blood samples were analyzed for ESR, CRP, ANA, ANCA, and anti-dsDNA, and a targeted next-generation sequencing (NGS) panel for autoinflammatory genes including TNFAIP3 was performed. Treatments received were recorded, including NSAIDs, glucocorticoids, colchicine, csDMARDs, bDMARDs, and other targeted therapies.
Results: Two patients (14.3%) had mutations identified via NGS: one in RIPK1 and another in PLCG2; no patient in our cohort tested positive for mutation in TNFAIP3. Both were Caucasian women with first-degree relatives affected by autoimmune disease, but had different ages of onset (29 vs. 5 years). Common symptoms included oral aphthae, arthralgia, abdominal pain, diarrhea, and fever. The RIPK1 case showed elevated fecal calprotectin and chest pain, without cutaneous or serologic abnormalities. The PLCG2 patient had acne, folliculitis, elevated acute phase reactants, and ANA positivity. Both received treatment with NSAIDs, and colchicine in the case of the RIPK1 patient. Cohort characteristics are summarized in Table 1.
Conclusion: In our cohort, despite recruiting patients with matching criteria for HA20, we found presence of two other mutations associated with autoinflammatory syndromes, not related to our target one. This remarks the importance of genetic testing when suspecting autoinflammation, specially in patients with no defined diagnosis, as it shows the clinical overlap between different entities. Identifying these distinct mutations could refine diagnosis and enable targeted treatment strategies by addressing underlying pathogenic mechanisms.
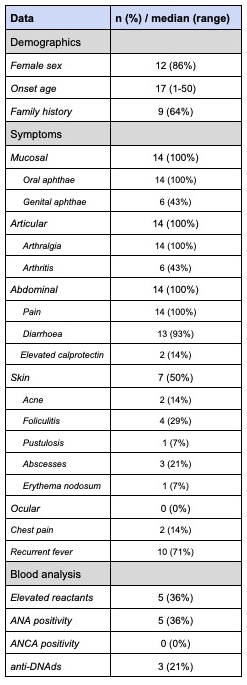 Table 1, part 1. Demographics, Symptoms, Blood Analysis
Table 1, part 1. Demographics, Symptoms, Blood Analysis
To cite this abstract in AMA style:
Alonso de Francisco M, González Vioque E, Navarro Palomo P, Machattou M, Navarro Joven C, Ramos Ortiz de Zarate L, Martínez A, Martín Bescós A, Mazo P, Sánchez Fernández M, Liso Andrino A, Barbadillo Mateos M, SANZ SANZ J, Godoy Tundidor H, Campos J, Fernandez Castro M, García Magallón B, Rusinovich O, Nuño L, Andreu J, Merino C. A20 Haploinsufficiency (HA20): TNFAIP3 Mutation Prevalence In A Clinically Compatible Cohort [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/a20-haploinsufficiency-ha20-tnfaip3-mutation-prevalence-in-a-clinically-compatible-cohort/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/a20-haploinsufficiency-ha20-tnfaip3-mutation-prevalence-in-a-clinically-compatible-cohort/

.jpg)