Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Social risk factors, such as housing instability, influence care access and outcomes in people with rheumatic conditions. In June 2022, 9 rheumatology clinics in a multihospital medical center began to screen patients for social risk factors. In September 2024, the Massachusetts Department of Public Health issued an alert of increased tuberculosis (TB) in Boston homeless shelters. Patients with systemic rheumatic conditions have higher TB infection risk and poorer outcomes; immunosuppressive medications heighten risk. We aimed to leverage the social risk screening infrastructure to rapidly respond to TB spread among homeless individuals with rheumatic conditions.
Methods: Using the Research Patient Data Registry and manual electronic health record (EHR) review, we identified patients with >1 ICD-9/10 code for a systemic rheumatic condition receiving >1 immunosuppressive or immunomodulatory medication who indicated that they did not have housing, lived in a shelter, or on the street on their most recent social risk screening. The rheumatology-based social risk screening team met with infectious disease (ID) specialists to develop protocols, and we alerted rheumatologists of patients at high risk for TB with a description of their patients’ risk factors, and instructions to screen for active and latent TB. We reviewed the EHR to determine provider response (Figure 1). If no action was taken, we sent a reminder. The EHR was reviewed after 2 months. Rheumatologists were surveyed for feedback.
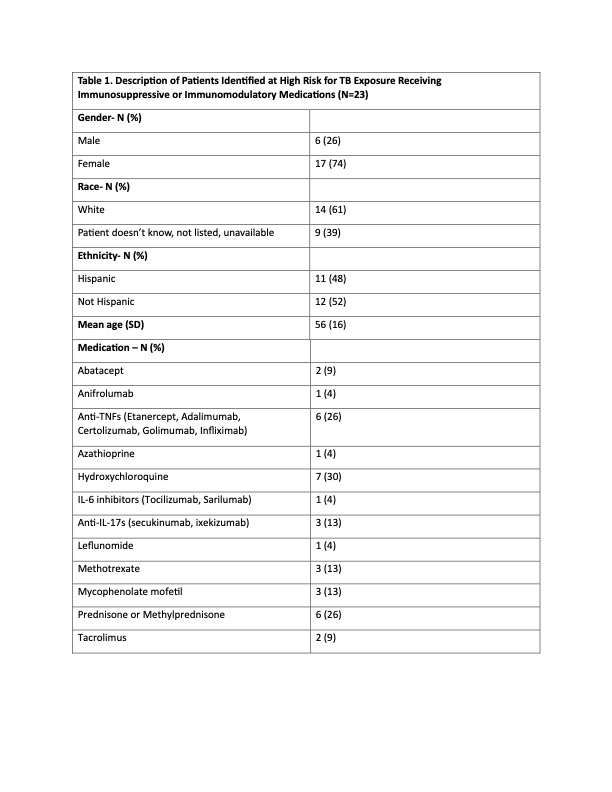
Results: Thirty-three patients with systemic rheumatic conditions experienced housing instability. Of these, 23 (70%) patients cared for by 17 rheumatologists were prescribed >1 immunosuppressive or immunomodulatory medication (Table 1). After the first alert, 3 (13%) patients had documentation of TB symptom screening, one provider responded that their patient was not homeless, and one ordered an interferon-gamma release assay (“T-SPOT”). Providers for two (9%) patients prescribed hydroxychloroquine were notified in case there was a therapy escalation plan, but a reminder was not sent due to lower risk. After the second alert, 7 (30%) T-SPOT tests were ordered. One patient self-reported a negative T-SPOT. Four (17%) patients had EHR documentation of symptom review at their subsequent rheumatology appointment, and 3 (13%) patients were messaged about their TB risk. Two (9%) patients had chest imaging ordered. There were no referrals to ID and no action taken for 4 patients. Among the 41 rheumatologists who responded to the survey, 18 (45%) received an alert for >1 patient. Of those, 4 (22%) found it somewhat helpful, 5 (28%) found it very helpful and 16 (89%) indicated that the alert prompted action.
Conclusion: The social risk screening infrastructure in rheumatology facilitated a rapid response to a public health concern. Rheumatologists’ responses varied, possibly due to increased clinical stressors with limited support. While there were challenges reaching patients with social risk factors, actions were taken for most. Efforts are now underway to prompt yearly TB screening for patients who indicate housing instability.
To cite this abstract in AMA style:
Summit R, Tierney D, Boadi T, Green T, Retzel K, Bills V, Shadick N, Santacroce L, Schoenfeld S, Feldman C. Leveraging Social Risk Factor Screening Infrastructure in Rheumatology Clinics to Respond to Rising Rates of Tuberculosis Among Individuals Experiencing Homelessness [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/leveraging-social-risk-factor-screening-infrastructure-in-rheumatology-clinics-to-respond-to-rising-rates-of-tuberculosis-among-individuals-experiencing-homelessness/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/leveraging-social-risk-factor-screening-infrastructure-in-rheumatology-clinics-to-respond-to-rising-rates-of-tuberculosis-among-individuals-experiencing-homelessness/

.jpg)