Session Information
Date: Sunday, October 26, 2025
Title: (0554–0592) Spondyloarthritis Including Psoriatic Arthritis – Treatment Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Previous studies have identified subgroups of patients with psoriatic arthritis (PsA) based on the severity of the disease [1,2]. However, no analysis to date has evaluated hidden pattern of PsA according to the peripheral manifestations and their influence on the response to TNF inhibitors (TNFi). The objectives of this study were: a) to identify clusters of PsA patients based on the presence of peripheral manifestations and psoriasis at the time of TNFi initiation, and b) to compare the effectiveness of the first TNFi across these clusters after 6 months of follow-up.
Methods: An observational, retrospective study was conducted in PsA patients naïve to TNFi. An unsupervised cluster analysis using the k-means technique was performed based on key peripheral features of PsA (arthritis, enthesitis, and dactylitis) and the presence of psoriasis. The response to TNFi treatment at 6 months (defined as ≥50% improvement in DAPSA) as well as achievement of DAPSA-LDA (DAPSA ≤ 14) and DAPSA-REM (DAPSA ≤ 4), were compared between clusters using the chi-square test.
Results: A total of 68 patients were included, 55.8% of whom were male, with a mean age of 50 years (SD 16.7) and a mean disease duration of 7.2 years. Two clusters were identified after the k-means analysis. Phenotypically, Cluster 1 (n=37) had a significantly lower prevalence of dactylitis (0% vs. 100%, p< 0.001) and psoriasis (64.9% vs. 90.3%, p=0.029) compared to cluster 2 (n=31) (Table 1). Other clinical variables at baseline, including mean swollen joint count (3.0 vs. 3.7, p=0.497) and tender joint count (6.0 vs. 5.4, p=0.628), were similar between clusters. However, CRP levels were significantly higher in Cluster 2 (21.4 vs. 8.5, p=0.049). No significant differences were found on the prevalence of concomitant csDMARDS (86.5% vs. 83.9%).After 6 months of TNFi treatment (Figure 1), the percentage of responders (defined as a ≥50% improvement in DAPSA) was numerically higher in Cluster 2 compared to Cluster 1, approaching statistical significance (35.1% vs. 58.1%, p=0.059). The proportion of patients achieving DAPSA-LDA was significantly greater in Cluster 2 (54.1% vs. 80.6%, p=0.021), while no significant difference was observed in DAPSA-REM rates between clusters.
Conclusion: Our findings suggest the presence of two distinct clinical phenotypes, primarily defined by the presence of dactylitis and psoriasis. Patients belonging to this phenotype had a higher likelihood of achieving low disease activity after 6 months of TNFi treatment. These results suggest that baseline phenotypic features may help predict treatment response.
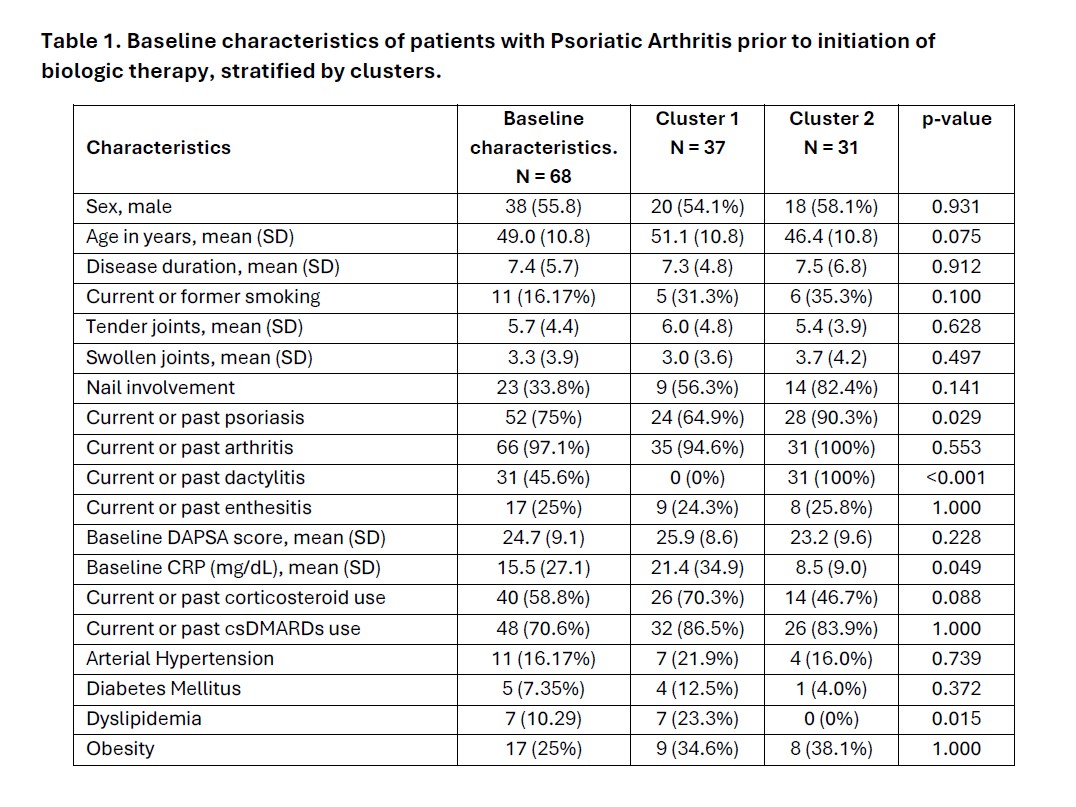 Table 1. Baseline characteristics of patients with Psoriatic Arthritis prior to initiation of biologic therapy, stratified by clusters.
Table 1. Baseline characteristics of patients with Psoriatic Arthritis prior to initiation of biologic therapy, stratified by clusters.
.jpg) Figure 1. Comparison of treatment response to TNF inhibitors between clusters after 6 months.
Figure 1. Comparison of treatment response to TNF inhibitors between clusters after 6 months.
To cite this abstract in AMA style:
Granados R, Martín Salazar J, Puche-Larrubia M, Ortiz Buitrago P, López-Montilla M, Calvo J, Ortega-Castro R, Romero-Gómez M, Escudero-Contreras A, Barbarroja N, López Medina C. Baseline Peripheral Phenotypes Are Associated with Differential Response to TNF Inhibitors in Psoriatic Arthritis. A Cluster Analysis Approach [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/baseline-peripheral-phenotypes-are-associated-with-differential-response-to-tnf-inhibitors-in-psoriatic-arthritis-a-cluster-analysis-approach/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/baseline-peripheral-phenotypes-are-associated-with-differential-response-to-tnf-inhibitors-in-psoriatic-arthritis-a-cluster-analysis-approach/
