Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Giant cell arteritis (GCA) is predominantly large vessel vasculitis that has a specific prediliction for vasculature of the head, eyes and jaw and if untreated can lead to permanent vision loss. The gold standard for diagnosis is a temporal artery biopsy (TABx) although only a portion of patients have a positive biopsy and the biopsy itself can be associated with additional morbidity. There is a significant need to more clearly understand the clinical features that are most specific to clinical presentation and positive biopsy as this has significant implications on treatment strategies.
Methods: We completed a single center large cohort (n=138) retrospective analysis of patients who underwent a TABx based on the clinical suspision for GCA. All biopsies were done within the Thomas Jefferson University Health System between August 2023 and June 2024. After IRB approval, chart review was completed to identify a variety of patient related characteristics including demographics, clinical features on presentation, lab and imaging results. Indepdent sample t-tests and both univariate and multivariate logistic regression models were used where appropriate to characterize differences between subjects with positive and negative TABx results.
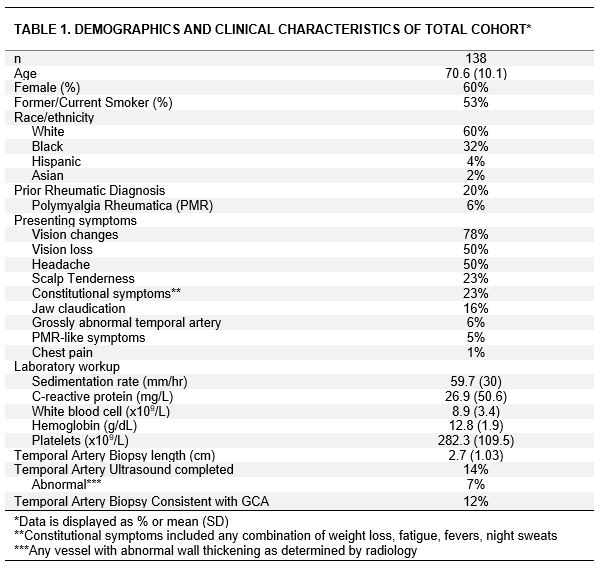
Results: The demographics and clinical features are summarized in table 1. The most common symptoms on presentation were vision changes (78%), vision loss (50%), temporal headache (50%) and scalp tenderness (23%). In 33% of patients, vision changes or vision loss was the only manifestation. The mean duration of steroid exposure prior to completion of biopsy was 3.8 days. The mean TABx length was 2.7 cm and a biopsy consistent with GCA was identified in 17/138 patients (12.1%). Of the 121 patients with a negative biopsy, 8 (6.6%) were treated for presumed GCA based on high clinical suspicion for the disease process. In simple logistic regression analysis, age (p< 0.01), jaw claudication (p< 0.01), grossly abnormal TA on exam (p=0.04), C-reactive protein (CRP) levels (0.04) and platelet count (0.05) were associated with increased odds of having a biopsy consistent with GCA (Table 2). In multivariate models, age, jaw claudication and platelet count remained independeltly significantly associated with odds of having a positive biopsy. Despite this, 3/17 (18%) patients with a positive TABx had 1) normal sedimentation rate (ESR) or CRP and 2) the only clinical feature on presentation was vision changes.
Conclusion: In this large retrospective analysis, we found several clinical features (age, jaw claudication, TA enlargement, CRP levels and platelet count) associated with pathology consistent with GCA with the most specific features being age, jaw claudication and increased platelets. A small portion of patients with a positive biopsy only exhibited vision changes and at least one normal inflammatory marker (ESR or CRP). Future studies are needed to more reliably characterize the full spectrum of the presentation of GCA and thus more expansive indications for invasive diagnostic studies such as a temporal artery biopsy.
To cite this abstract in AMA style:
Perdomo w, Welch S, Wilson T. Diagnostic Utility of Temporal Artery Biopsy in Giant Cell Arteritis: A Single Center Experience [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/diagnostic-utility-of-temporal-artery-biopsy-in-giant-cell-arteritis-a-single-center-experience/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/diagnostic-utility-of-temporal-artery-biopsy-in-giant-cell-arteritis-a-single-center-experience/

.jpg)