Session Information
Date: Sunday, October 26, 2025
Title: (0731–0764) Vasculitis – Non-ANCA-Associated & Related Disorders Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Giant cell arteritis (GCA) is the most common vasculitis in patients 50 years and older. Glucocorticoids (GC) are the mainstay of treatment for GCA but can cause significant adverse events (AE). This study assessed GC burden, treatment patterns and rheumatologists’ perceptions of advanced therapies (AT) for GCA.
Methods: Data were from the Adelphi Real World GCA Disease Specific ProgrammeTM, a cross-sectional, retrospective survey of rheumatologists and their adult (≥18 years) patients with GCA in France, Germany, Italy, Spain, and the United Kingdom (EU-5), and the United States (US) from 05/2024–10/2024. Rheumatologists completed patient record forms (PRF) for each patient to record demographics, treatment history and clinical characteristics. Rheumatologists were surveyed on their patient management approach and treatment perceptions. Patients for whom a PRF was completed were invited to fill in a self-assessment form.
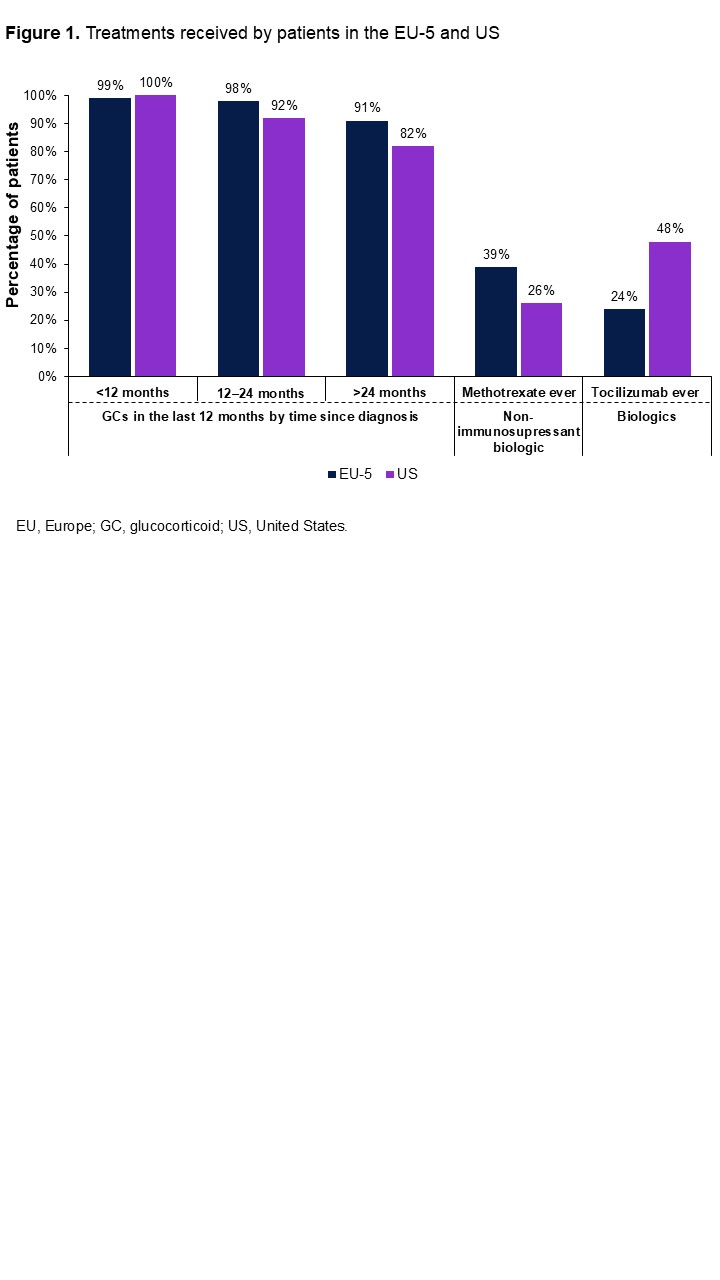
Results: Overall, 189 rheumatologists were surveyed. Among 846 patients with GCA (EU-5: France, Nf133; Germany, Nf120; Italy, Nf144; Spain, Nf120; UK, Nf129; US: Nf200), 63% were female, 94% were white, mean age was 71 years and median time since diagnosis was 15.2 months. Most patients were using GCs, regardless of time since diagnosis. The next most common treatments were tocilizumab (EU-5, 24%; US, 48%) and methotrexate (EU-5, 39%; US, 26%; Figure 1). Median time from diagnosis to receiving tocilizumab or methotrexate was approximately 5 months. Over the last 12 months, median cumulative GC doses were 4343 mg, 5200 mg and 2196 mg for patients diagnosed < 1 year, 1–2 years, and >2 years ago, respectively. Most rheumatologists (87%) aimed to taper to low dose GCs by 12 months and 79% aimed to taper off GCs completely by 24 months post-diagnosis. At 24–< 36 months post-diagnosis, 80% of patients were on an average daily GC dose of 8.4 mg, and 75% were taking an average of 5.3 mg/day at ≥48 months (Figure 2). The number of patients experiencing ≥1 GC-related AE was higher when reported by rheumatologists (74%) compared to patients (55%; Figure 3). Most rheumatologists (EU-5, 90%; US, 94%) agreed that ATs should be given early in GCA treatment to improve outcomes and reduce GC toxicity. Over 90% of rheumatologists believed the following AT attributes were important: maintenance of remission; achievement of GC-free remission; reduction of high-dose/cumulative GC use; to allow GC cessation; and to be safe, tolerable, and patient-compliant. Most rheumatologists agreed that limited choices in AT administration routes are a barrier to widespread use (EU-5, 51%; US, 80%) and that convenient administration is an important attribute of ATs (EU-5, 65%; US, 84%). Most patients (75%) stated that they preferred receiving treatments orally rather than by injection or infusion.
Conclusion: Even though most rheumatologists aimed to taper patients off GCs completely by 24 months, 75% of patients were using GCs at 4 years. Both rheumatologists and patients reported several AEs associated with GC use, and rheumatologists recognize the need for early and effective steroid sparing intervention with ATs.
To cite this abstract in AMA style:
Dua A, Kadakia A, Zueger P, Marwaha S, Zerad N, Setty A, Jones W, Devauchelle V. Real World Steroid Burden, Treatment Patterns, and Rheumatologists’ Perceptions on Advanced Therapy in Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/real-world-steroid-burden-treatment-patterns-and-rheumatologists-perceptions-on-advanced-therapy-in-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/real-world-steroid-burden-treatment-patterns-and-rheumatologists-perceptions-on-advanced-therapy-in-giant-cell-arteritis/

.jpg)
.jpg)