Session Information
Date: Sunday, October 26, 2025
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Axial involvement in psoriatic arthritis (axPsA) is associated with more severe disease and greater pain compared to PsA with only peripheral disease. However, a consensus definition of axPsA is lacking, complicating diagnosis and treatment. This study aims to describe the occurrence and characteristics of MRI and radiographic sacroiliac joint (SIJ) involvement in a European cohort of patients with PsA.
Methods: Patients with a clinical diagnosis of PsA (clin-PsA) or axial spondyloarthritis with psoriasis (axSpA+Pso), who had available routine care SIJ MRIs and clinical data, were included from five European registries in the EuroSpA collaboration. SIJ MRIs and radiographs were centrally evaluated by two experienced readers for inflammatory and structural lesions, differential diagnoses, and a global assessment for SpA-indicative findings. Disagreements were adjudicated by a third expert reader. Associations between MRI-detected axPsA (defined as MRI findings indicative of SpA) and clinical characteristics were analysed using logistic regression with multiple imputations for missing data.
Results: Among the 581 included patients (Clin-PsA: n=373; axSpA+Pso: n=208), 47% were male, with a mean age of 45 years (Table 1). At the time of MRI examination, 76% had not received biological treatment. In 31% of patients, MRI findings were indicative of SpA (MRI-axPsA). Inflammatory SpA-indicative lesions were present in 21% of patients, and structural lesions in 28%, with 76% of affected patients having both lesion types. Common differential diagnoses included osteitis condensans ilii (8%), probable strain-related bone marrow edema (BME) (11%), and degenerative changes (16%). In 35% of patients, SIJ MRIs were normal, showing no SpA-related lesions or alternative diagnoses. Among patients with MRI-axPsA the SIJ MRI findings were predominantly bilateral, with BME (69%), erosion (68%), and fat lesions (58%) being the most common. BME (≥1 cm), inflammation in an erosion cavity, capsulitis, fat lesions (≥1 cm), backfill, and ankylosis were observed almost exclusively in this group (Figure 1). Among 259 patients with available radiographs, 29% met the radiographic component of the modified New York criteria (r-mNYc) for ankylosing spondylitis, while 38% had an MRI indicative of SpA. Radiographic SIJ involvement was predominantly bilateral (91%) in patients meeting the r-mNYc.Male sex, HLA-B27 positivity, elevated CRP and history of inflammatory back pain, but not current back pain were independently associated with MRI-AxPsA, while peripheral arthritis showed a negative association. Various clinical, radiographic, and MRI-based definitions of axial PsA were applied and compared (Table 2), using overall MRI findings indicative of SpA as the reference (Table 1, 5. MRI ‘global’ definition). No clinical or radiographic definition performed similarly to this MRI definition.
Conclusion: In this large European cohort, approximately one-third of routine care PsA patients had an SIJ MRI indicative of SpA. Integrating MRI into future axPsA definitions may facilitate earlier detection, and guide treatment choices in clinical practice.
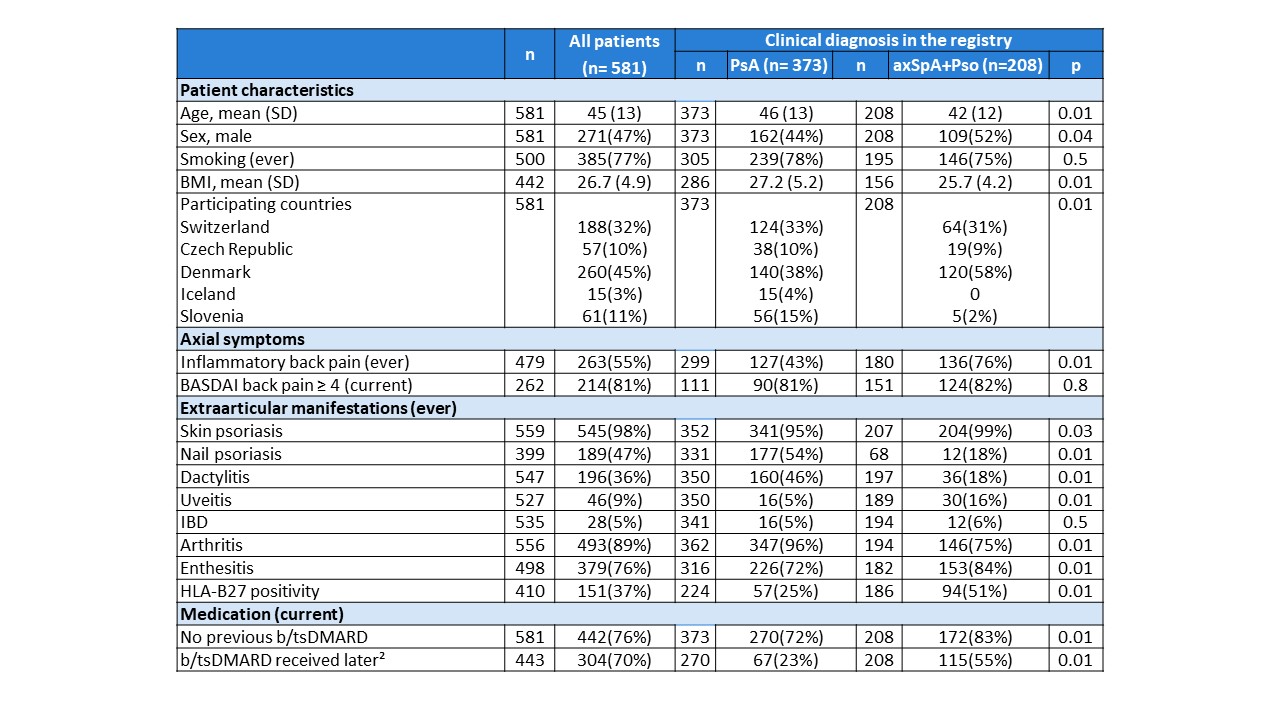 Table 1. Patient characteristics
Table 1. Patient characteristics
P-value < 0.05 is considered significant, Chi-squared test or Fisher’s test are used for categorical variables, t-test or Wilcoxon rank-sum test for continuous variables. All variables are presented as n (%) unless indicated. For each variable, available data (n) are presented in separate column (n) for all patients and for each subgroup.
Pso-AxSpA: Psoriasis and axial spondyloarthritis; clin-PsA: Peripheral psoriatic arthritis; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; HLA-B27: human leucocyte antigen-B27;
¹b: biological, ts: targeted synthetic Disease modifying antirheumatic drug (DMARD) received prior to or at the time of MRI examination; ²b/tsDMARD initiated such treatment at some point after the MRI examination.
.jpg) Figure 1. Inflammatory and structural MRI lesions in PsA patients with an MRI indicative of SpA (MRI-AxPsA group) versus not indicative of SpA (MRI-noAxPsA)
Figure 1. Inflammatory and structural MRI lesions in PsA patients with an MRI indicative of SpA (MRI-AxPsA group) versus not indicative of SpA (MRI-noAxPsA)
BME, bone marrow edema; Infl Ero cav, inflammation in an erosion cavity; Confl Ero, confluent erosion; Fat, fat lesion
.jpg) Table 2. Fulfilment of various definitions of axial psoriatic arthritis in all patients and in patients with (MRI-AxPsA) versus without (MRI-noAxPsA) MRI findings indicative of SpA
Table 2. Fulfilment of various definitions of axial psoriatic arthritis in all patients and in patients with (MRI-AxPsA) versus without (MRI-noAxPsA) MRI findings indicative of SpA
MRI-AxPsA: patients with SIJ MRI findings indicative of SpA at the global SIJ MRI assessment; MRI-noAxPsA: patients without SIJ MRI findings indicative of SpA at the global SIJ MRI assessment. ASAS: Assessment of SpondyloArthritis International Society; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; mNY criteria: Modified New York criteria for ankylosing spondylitis
To cite this abstract in AMA style:
Vladimirova N, Hadsbjerg A, Krabbe S, Ciurea A, Bubová K, Gregova M, Nissen M, Moeller B, Micheroli R, Pedersen S, Zavada J, Snoj Z, Pintaric K, Gudbjornsson B, Rotar Z, Eshed i, Iwona Sudol-Szopinska I, Gosvig K, Diekhoff T, Lambert R, de Hooge M, Donzallaz M, Bernatschek A, Hetland M, Ørnbjerg L, Ostergaard M. Unveiling Sacroiliac Joint Involvement in Psoriatic Arthritis: MRI, Radiographic, and Clinical Insights from 581 European Routine Care Patients [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/unveiling-sacroiliac-joint-involvement-in-psoriatic-arthritis-mri-radiographic-and-clinical-insights-from-581-european-routine-care-patients/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/unveiling-sacroiliac-joint-involvement-in-psoriatic-arthritis-mri-radiographic-and-clinical-insights-from-581-european-routine-care-patients/
