Session Information
Date: Sunday, October 26, 2025
Title: (0337–0356) Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Osteoporosis treatment is essential to prevent fractures. However, few patients with proximal femur fractures receive osteoporosis treatment before injury. Initiating treatment postoperatively is critical to reduce the risk of subsequent fractures, such as contralateral hip and vertebral fractures. Our institution proactively initiates osteoporosis treatment during hospitalization after proximal femur fracture surgery. We perform bone mineral density measurements, spinal and pelvic X-rays, and blood tests, including bone turnover markers, to guide medication selection. Although bone turnover markers should ideally be measured within 24 hours of injury, postoperative measurement is sometimes unavoidable. This study evaluated differences in blood test parameters between pre- and postoperative periods, assessed differences by fracture type, and examined considerations when bone turnover markers cannot be measured early.
Methods: We included 179 patients (41 males, 138 females; mean ages 82.6, 82.8 years) hospitalized within 24 hours of a proximal femur fracture. Of these, 81 had femoral neck fractures (18 males, 63 females; mean ages 82.5, 82.7), and 98 had trochanteric fractures (23 males, 75 females; mean ages 82.9, 83.0).All patients underwent preoperative blood tests at admission, followed by surgery (osteosynthesis, bipolar hip arthroplasty, or total hip arthroplasty). We measured procollagen type 1 N-terminal propeptide (P1NP), tartrate-resistant acid phosphatase-5b (TRACP-5b), 25-hydroxyvitamin D, alkaline phosphatase, calcium, and phosphorus at admission and 1–2 weeks postoperatively. Changes before and after surgery, and differences by fracture type, were analyzed using t-tests.
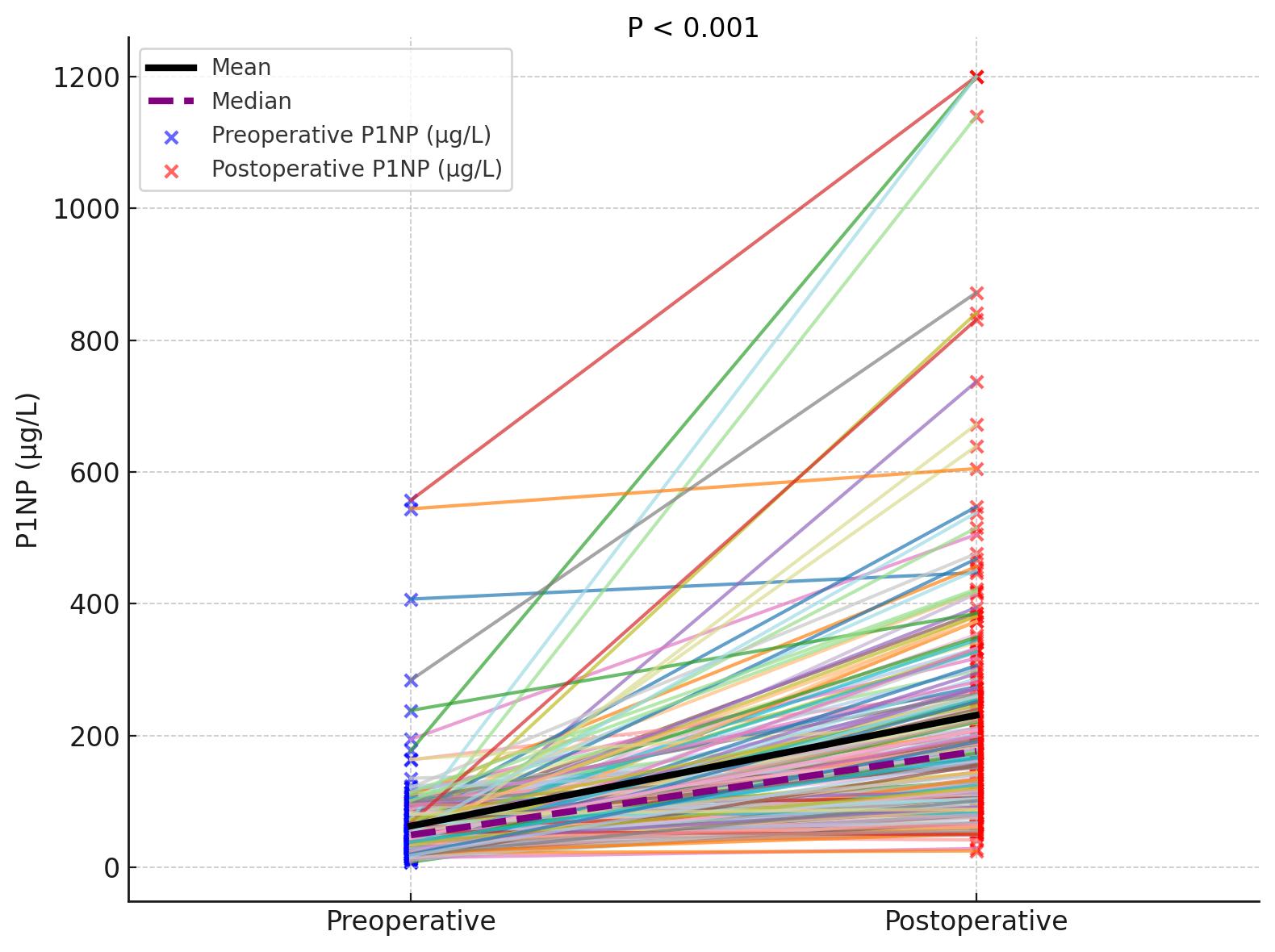
Results: Postoperative P1NP levels increased in 171 of 179 patients (76 of 81 femoral neck, 95 of 98 trochanteric fractures), averaging a 3.7-fold increase. Preoperative 25-hydroxyvitamin D levels were < 20 ng/mL in 163 patients (76 femoral neck, 87 trochanteric), declining further postoperatively in 170 patients (78 femoral neck, 92 trochanteric). A postoperative decrease was seen in 137 patients (63 femoral neck, 74 trochanteric). Significant differences (P < 0.001) were observed in P1NP and 25-hydroxyvitamin D between pre- and postoperative measurements, regardless of fracture type. No significant changes were seen in TRACP-5b, alkaline phosphatase, calcium, or phosphorus, and no fracture type differences were detected.
Conclusion: We observed a marked postoperative increase in P1NP, highlighting the importance of early measurement to avoid overestimation due to fracture-induced elevation. These findings were consistent across fracture types, supporting uniform management. When early assessment is not feasible, clinicians should interpret P1NP cautiously and consider alternative markers, recognizing that elevated P1NP alone should not preclude anabolic therapy. The postoperative decline in 25-hydroxyvitamin D underscores the need for early active vitamin D supplementation. These findings provide practical guidance for optimizing osteoporosis management in acute fracture care.
To cite this abstract in AMA style:
NAKASEKO K. Perioperative Evaluation of Blood Tests Including Bone Turnover Markers in Patients Undergoing Surgery for Proximal Femur Fractures [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/perioperative-evaluation-of-blood-tests-including-bone-turnover-markers-in-patients-undergoing-surgery-for-proximal-femur-fractures/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/perioperative-evaluation-of-blood-tests-including-bone-turnover-markers-in-patients-undergoing-surgery-for-proximal-femur-fractures/

.jpg)