Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Presence of high titer antiphospholipid antibodies (aPLs) confer adverse pregnancy outcomes (APOs). Patients with low titer aPLs often receive conflicting counseling on treatment, many are treated with dual antiplatelet and low molecular weight heparin (LMWH) therapy without clear benefit. We conducted a pilot study to investigate the association of low profile aPLs and APOs.
Methods: We performed a retrospective cohort study using electronic health record (EHR) data of all pregnant women who received aPL testing and hospitalized in a major tertiary care center from 2013 to 2022. Women were categorized into three exposure groups: (1) negative aPLs: anti-cardiolipin ± anti-b2- glycoprotein IgG, IgA, or IgM < 20 GPL/MPL; (2) low profile aPLs, defined as anti-cardiolipin ± anti-ß2- glycoprotein IgG, IgA, or IgM 20-39 GPL/MPL; (3) high profile aPLs, defined as anti-cardiolipin ± anti-ß2- glycoprotein IgG, IgA, or IgM ≥40 GPL/MPL, and/or presence of lupus anticoagulant. The outcomes of interest were: (1) late pregnancy losses and stillbirths; (2) pre-eclampsia and eclampsia. Next, we performed logistic regression to determine the exposure-outcome associations in the low profile aPLs group. The analyses were adjusted for age, parity, obesity, co-morbidities including rheumatic diseases, hypertensive disorders, diabetes, history of recurrent pregnancy losses, aspirin and LMWH use.
Results: We included 2,133 women who were hospitalized during the latter part of pregnancy and tested for aPLs. < 10% of women had positive aPLs and among those, almost half of these women were considered low profile. The mean age of women with low and high profile aPLs was the same (33.7 years of age), Caucasian women constitute more than half in all groups. Most women had private insurance (Nf1218; 57.1%). Several conditions were most prevalent in the high-profile group, including obesity (Nf56, 56.6%), hypertensive diseases during pregnancy (Nf27, 27.3%), and rheumatic diseases (Nf41, 41.4%). Women with low profile aPLs were more likely to have history of recurrent pregnancy losses (Nf34, 35.4%); smoking (Nf150, 7.7%) during pregnancy was most frequent among negative aPL group (Table 1). Among women with low profile aPLs, the adjusted Odds Ratio (aOR) of pre-eclampsia and eclampsia compared to negative aPL group was 0.92 (95%CI 0.49, 1.66; p=0.792), and the aOR of late pregnancy loss and stillbirths was 0.51(95%CI 0.20, 1.11; p=0.092) (Table 2).
Conclusion: In the low profile group, the odds of developing the APOs of interest were lower or similar, compared to those with negative aPLs despite treatment with aspirin or LMWH. Women with negative aPLs may be more ill and therefore required inpatient care in this study sample. The limitations of this pilot study include small sample sizes, potential selection bias, and incomplete ascertainment of specific variables. Our findings may not be representative of the general population, but the associations of this pilot study inform additional EHR data collection to improve the limitations above. Future work would include the use of propensity score weighting to account for confounding and to balance the characteristics among groups.
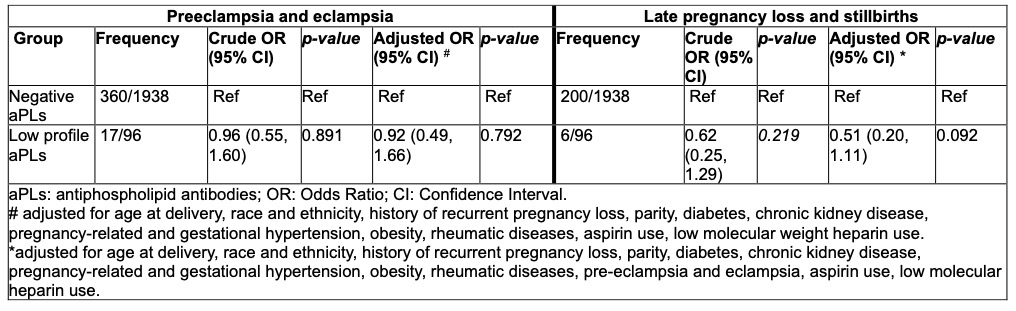 Table 1. Characteristics of study population by aPL profile.
Table 1. Characteristics of study population by aPL profile.
.jpg) Table 2. Risks of adverse pregnancy outcomes among women with low aPLs.
Table 2. Risks of adverse pregnancy outcomes among women with low aPLs.
To cite this abstract in AMA style:
Chock E, Wang T, Memon A, Liew Z, Guo P. The role of low profile antiphospholipid antibodies and adverse pregnancy outcomes. [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/the-role-of-low-profile-antiphospholipid-antibodies-and-adverse-pregnancy-outcomes/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-role-of-low-profile-antiphospholipid-antibodies-and-adverse-pregnancy-outcomes/
