Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Brucellosis, one of the most prevalent zoonotic diseases worldwide, often results in osteoarticular complications including large joint and axial arthritis mimicking spondyloarthritis (SpA). Greater understanding of Brucella SpA may reveal common mechanisms with rheumatologic SpA and yield insight into how host-pathogen interactions drive SpA. As previous Brucella mouse models were problematic, we developed a new one using SpA susceptible SKG mice. In this study, in addition to initial characterization of the model, we sought to determine if Brucella SpA reflected persistent infection or a reactive process.
Methods: SKG mice of both sexes were infected with various species of Brucella varying in human virulence and monitored for weight loss, arthritis (score and changes in paw widths), eye inflammation and rash for 12 weeks. New bone formation was detected by micro-CT. Viable infection was assessed by colony forming units (CFU) in paws and spleen and in vivo imaging (IVIS) of luminescent Brucella.
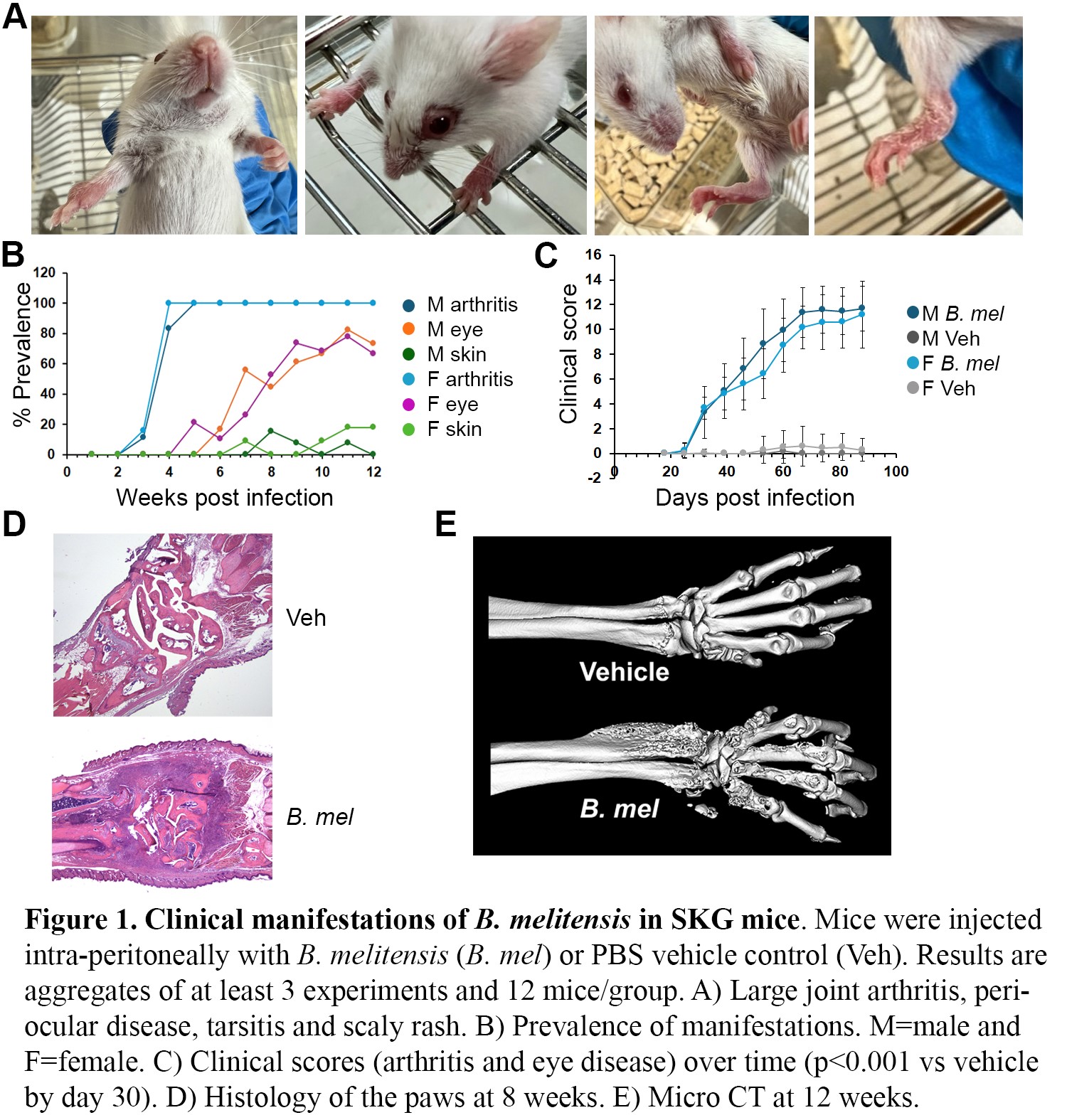
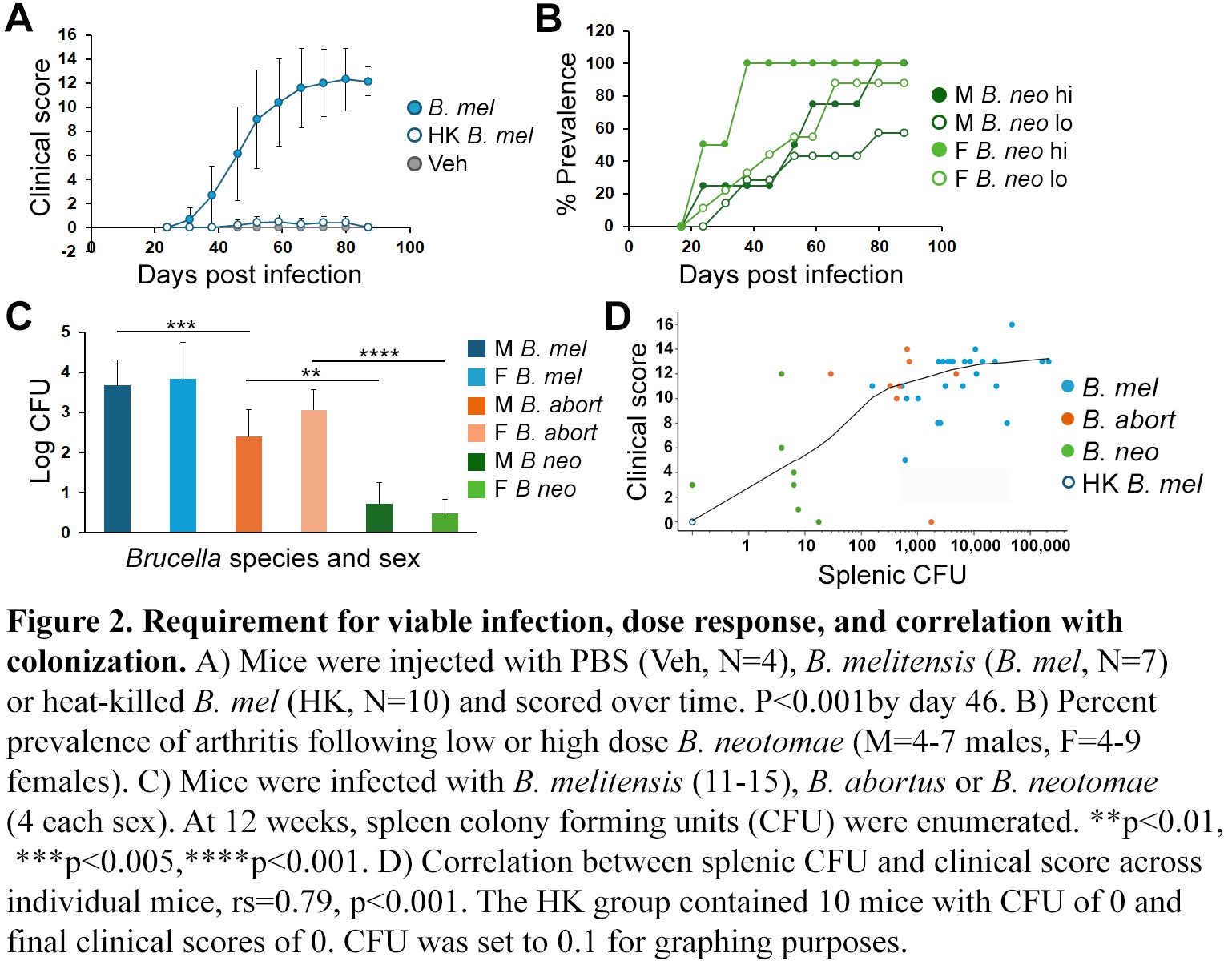
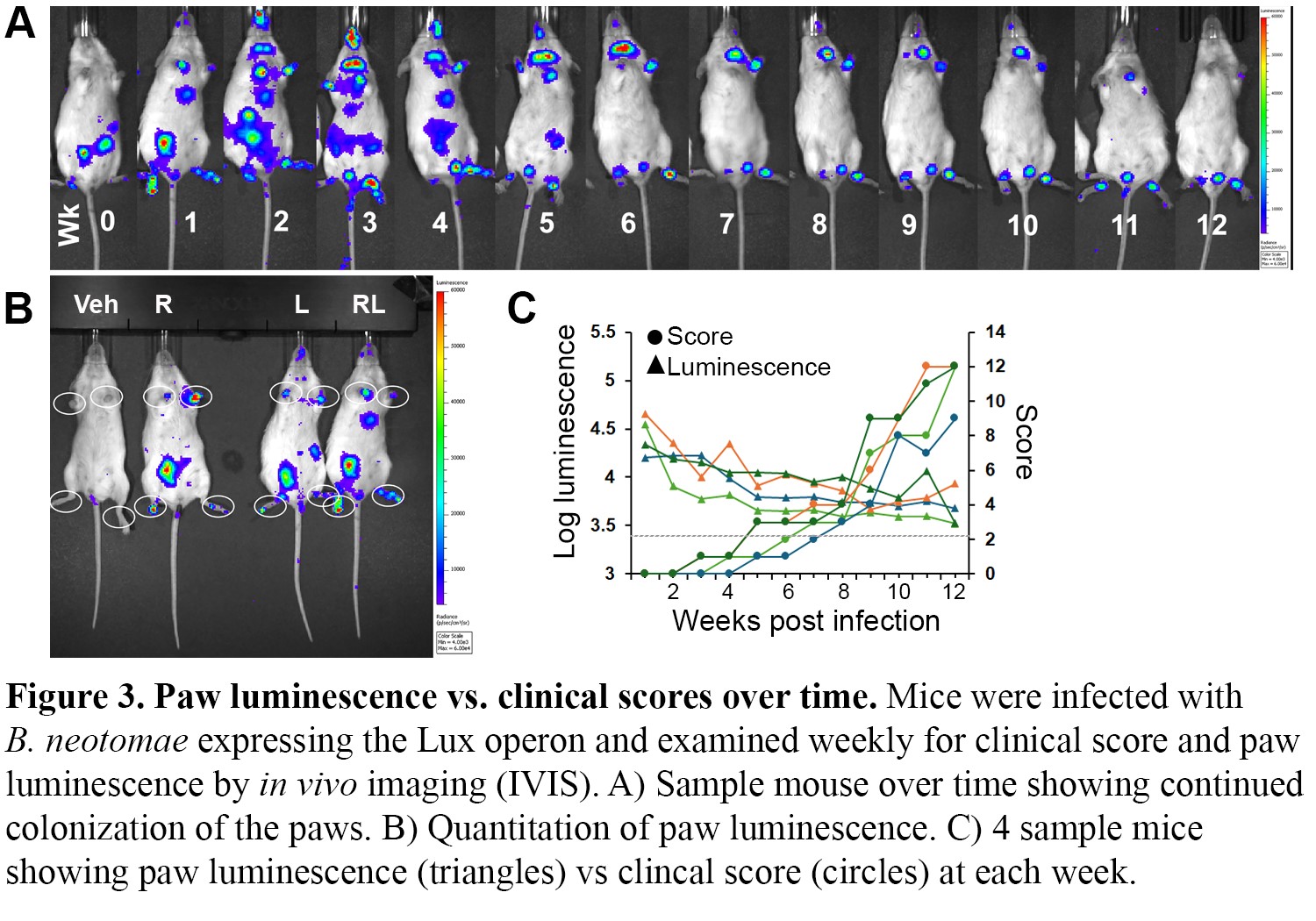
Results: B. melitensis infection resulted in fully penetrant, readily scoreable disease involving large joint wrist and foot arthritis, peri-ocular inflammation, occasional scaly paw rash, and florid new bone formation (Figure 1). B. abortus elicited more variable disease, and B. neotomae revealed sex differences, with more penetrant and severe disease in females. Heat-killed Brucella did not induce arthritis, evincing a requirement for viable infection. Also, the prevalence and severity of B. neotomae disease exhibited a dose response. Splenic CFU correlated well with final clinical score at 12 weeks (rs=0.79 and p< 0.001, Figure 2). On the other hand, in vivo imaging using luminescent B. neotomae revealed rapid colonization of the paws by one week post-infection, more than a month prior to arthritis onset. Luminescence levels decreased after 2 weeks and then remained relatively static, even as clinical scores increased (Figure 3). Thus, the degree of arthritis did not strictly correlate with degree of paw infection but suggested an additional reactive component. Further, in examining a Brucella ΔTcpB mutant lacking a Type IV secretion system-dependent effector, mice displayed an intermediate arthritis phenotype without significant differences in splenic CFU.
Conclusion: Together these data suggest Brucella induced SpA reflects both persistent colonization as well as excess host reactivity. Moreover, the sensitivity of the SKG model to different bacterial species and mutants will provide new opportunities for dissecting the correlates of Brucella virulence and the host immunity that drive the development of SpA.
To cite this abstract in AMA style:
Harms J, Eickhoff J, Warner T, Smith J. Persistent Articular Infection and Host Reactive Responses Contribute to Brucella-Induced Spondyloarthritis in SKG Mice [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/persistent-articular-infection-and-host-reactive-responses-contribute-to-brucella-induced-spondyloarthritis-in-skg-mice/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/persistent-articular-infection-and-host-reactive-responses-contribute-to-brucella-induced-spondyloarthritis-in-skg-mice/