Session Information
Date: Monday, November 18, 2024
Title: Abstracts: Vasculitis – Non-ANCA-Associated & Related Disorders II
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: There is a need for measures of disease severity for giant cell arteritis (GCA), which may enable identification of high-risk subgroups (e.g., ophthalmic complications) and allow for individualized approach to therapy. Cranial vessel wall MRI (VW-MRI) has potential to quantify disease severity by detecting inflammation of multiple cranial arteries beyond the temporal arteries. We hypothesize a greater extent of vascular inflammation predicts ocular manifestations of GCA, including MRI enhancement of orbital structures, which has been previously demonstrated to potentially detect subclinical orbital disease in GCA. In this study, we derived a continuous score to quantify GCA disease severity based on extent of abnormal enhancement on VW-MRI and assessed the score’s association with: i) diagnosis, ii) ophthalmologic manifestations of GCA and iii) orbital enhancement on MRI.
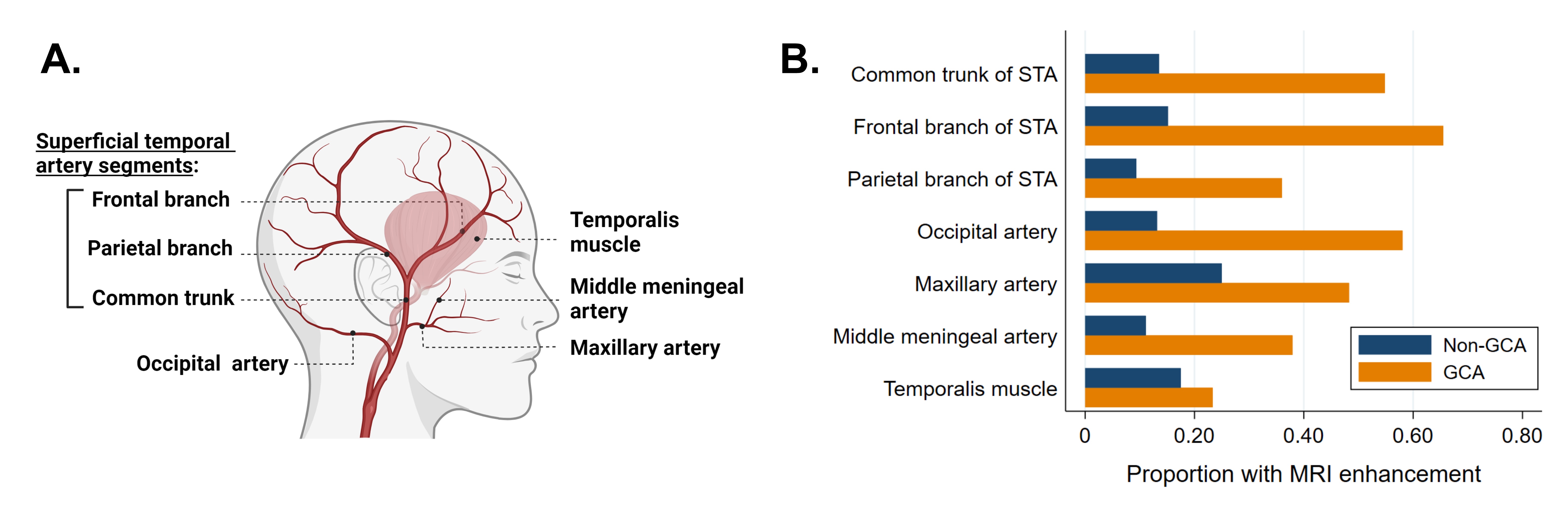
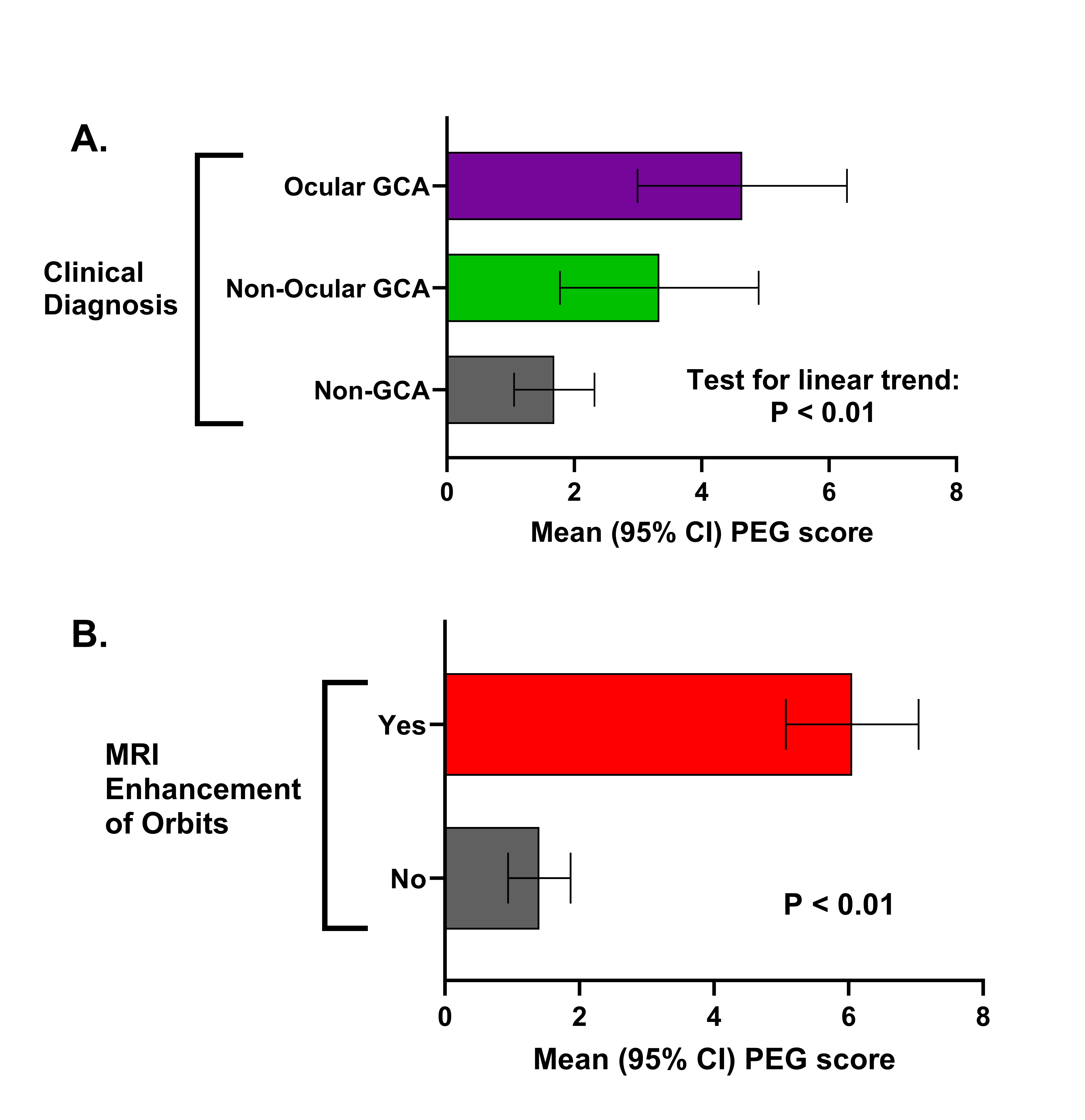
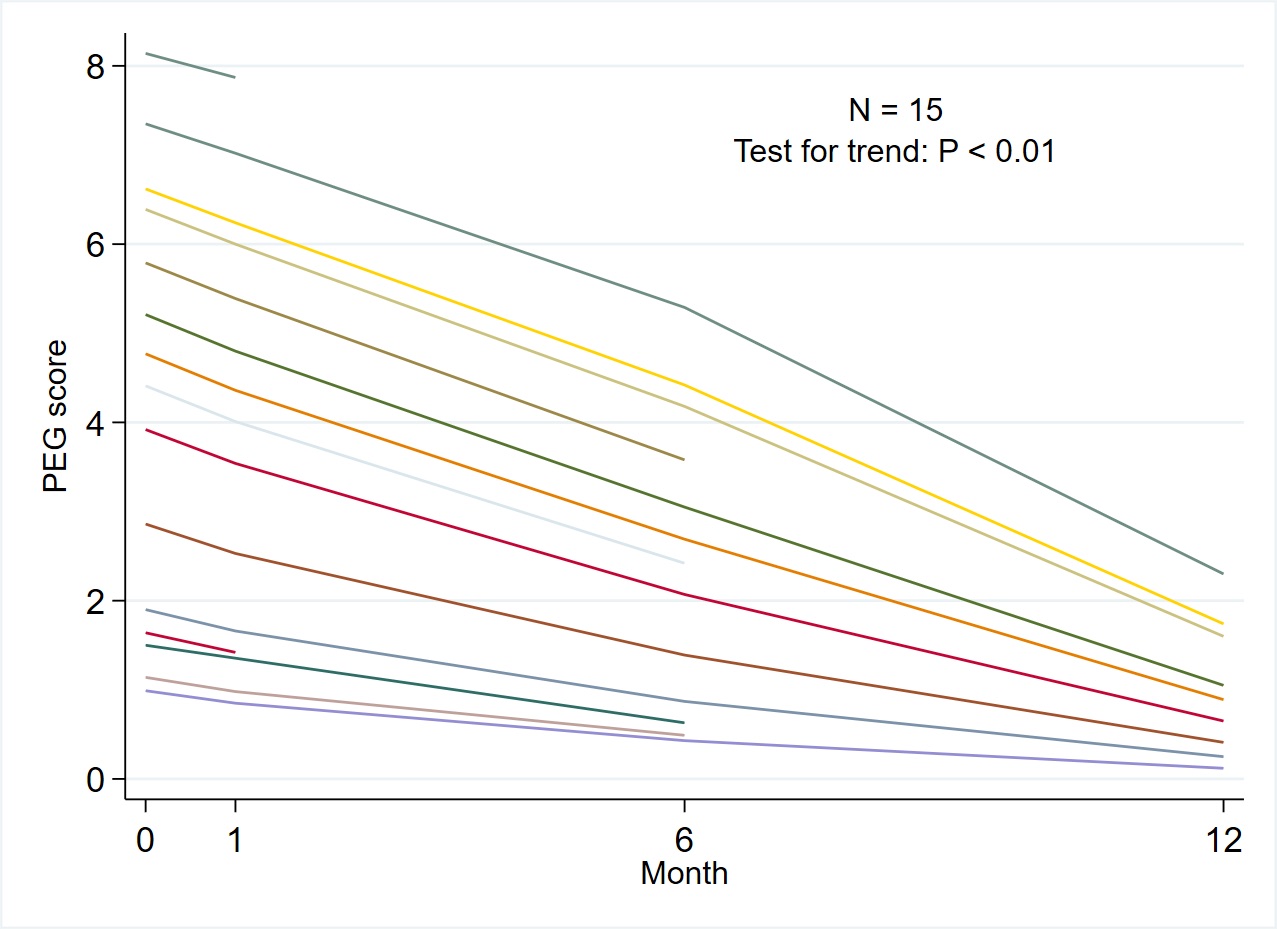
Methods: Patients with suspected new or relapsing GCA who underwent cranial and orbital VW-MRI were included. A subset of patients received repeat MRIs at month 1,6, and 12. Patients were clinically diagnosed as ocular GCA, non-ocular GCA, or non-GCA. A radiologist assessed MRI enhancement of 7 structures bilaterally (Figure 1A). Orbital enhancement on MRI was defined as enhancement of ophthalmic artery or optic nerve sheath. Using a generalized linear mixed effects model with sum-to-zero contrasts, scorable MRI structures (excluding orbital structures) were used to derive a continuous patient-level score representing disease extent. The score, named the Propensity for Enhancement for GCA (PEG) score, ranges from 0 (no enhancement) to 10 (maximum enhancement), accounts for missing arteries, and adjusts for arteries with higher propensities for enhancement. The PEG score was compared between groups using Wilcoxon rank-sum test or linear trend test.
Results: Seventy-five patients (17 ocular GCA, 16 non-ocular GCA, and 42 non-GCA) were included. GCA patients had a greater proportion of structures with abnormal MRI enhancement compared to non-GCA patients. (Figure 1B). PEG score linearly increased across clinical subgroups of non-GCA, non-ocular GCA, and ocular GCA (test for trend: P < 0.01; Figure 2A). Orbital MRI enhancement was observed in 18 (55%) GCA patients including 12 (71%) ocular GCA patients and 6 (38%) with non-ocular GCA. Mean PEG scores were higher in the group with vs. without orbital MRI enhancement (0.61 [0.22] vs. 0.14 [0.17], p< 0.01, Figure 2B). For 15 patients with GCA who underwent repeat MRIs, the PEG score decreased over time with treatment (Figure 3).
Conclusion: VW-MRI reveals the extent of cranial vascular inflammation in GCA patients and is associated with clinical and imaging manifestations of ophthalmic GCA. The PEG score, a novel measure derived from the additive effect of abnormally enhancing MRI structures, is higher in GCA patients with visual manifestations and patients with orbital MRI enhancement. PEG scores improve with treatment. Assessing multiple cranial arteries using VW-MRI may improve assessment of GCA disease severity, which could inform treatment decision-making and clinical trial design.
To cite this abstract in AMA style:
Yang D, Cao Q, Liu F, McWilliams T, Rebello R, Tamhankar M, Banerjee S, Liang R, Kurtz R, Baker J, Amudala N, Fan Z, Song J, Merkel P, Morris J, Rhee R. Extent of Vascular Inflammation on Cranial Vessel Wall MRI and Ophthalmic Complications in Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/extent-of-vascular-inflammation-on-cranial-vessel-wall-mri-and-ophthalmic-complications-in-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/extent-of-vascular-inflammation-on-cranial-vessel-wall-mri-and-ophthalmic-complications-in-giant-cell-arteritis/