Session Information
Date: Monday, November 18, 2024
Title: Abstracts: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Osteoporosis remains poorly identified and treated. We studied the effects of an organized osteoporosis program of care on treatment rates over a 20-year period.
Methods: In 2008, we built an osteoporosis program with consultative DXA reporting, reliable identification of high-risk patients, and in/outpatient osteoporosis services. A retrospective study examined 3- and 5-year treatment trends in our osteoporosis population through seven 3-year time periods, 2002-2022. Eligibility criteria had patients ≥50 years with ≥1 PCP visit and ≥1 high risk DXA in each period. 3-year therapy was defined as patient on active or having ≥3-years of treatment in each period. 5-year therapy was defined as active or having ≥5 years of treatment. Active therapy was defined as on oral bisphosphonate or anabolic by period end date, denosumab within the last 8-months, or zoledronate in the last 14-months of the period. Treatment comparisons were made by insurance, visit type (PCP vs non-PCP) race, age, and gender. The non-PCP group involved specialty [Rheumatology or Endocrinology] clinic and osteoporosis clinic. A sub-analysis compared treatment rates of our osteoporosis clinic to the PCP and specialty group. Chi-square or Fisher exact tests were used.
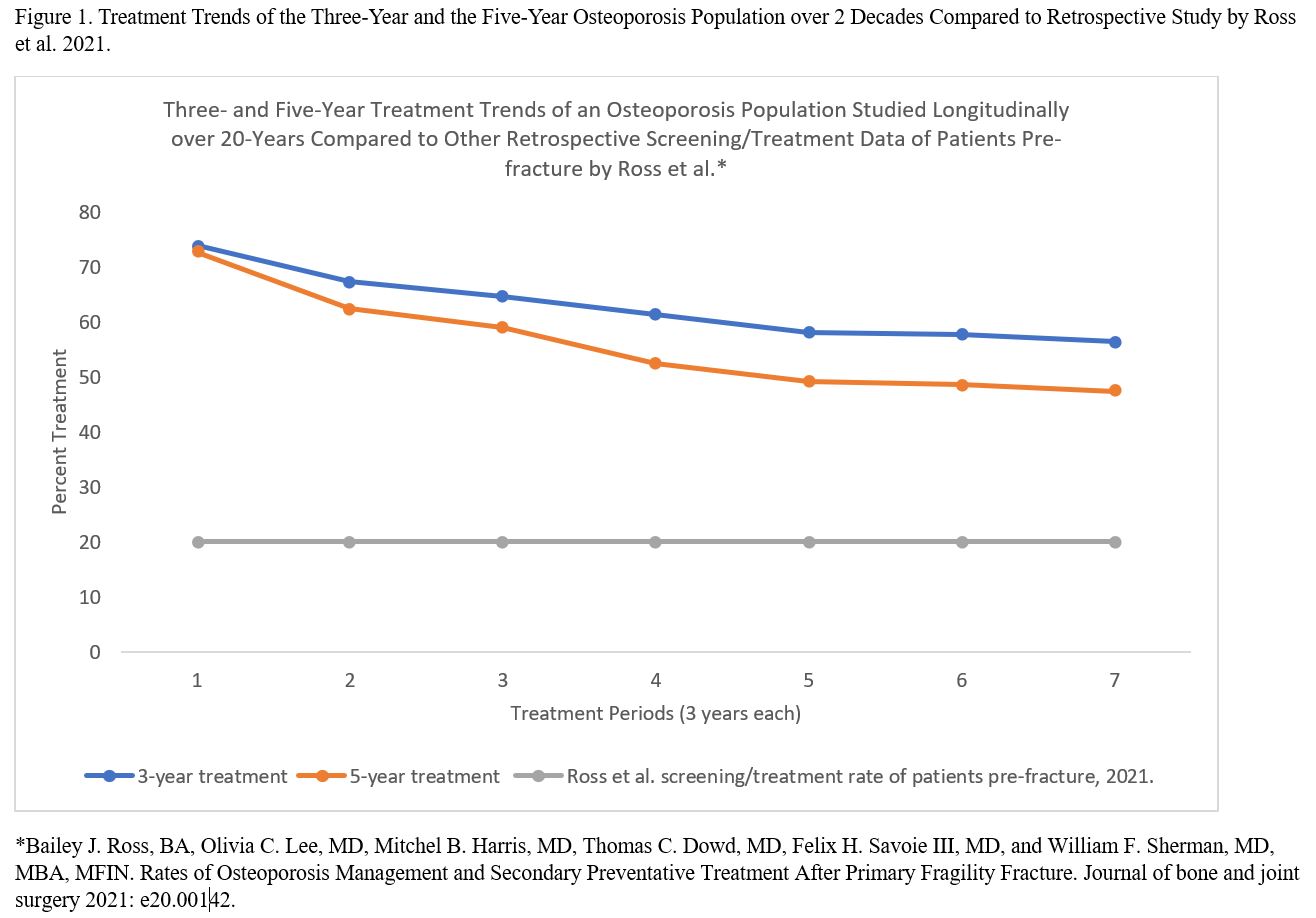
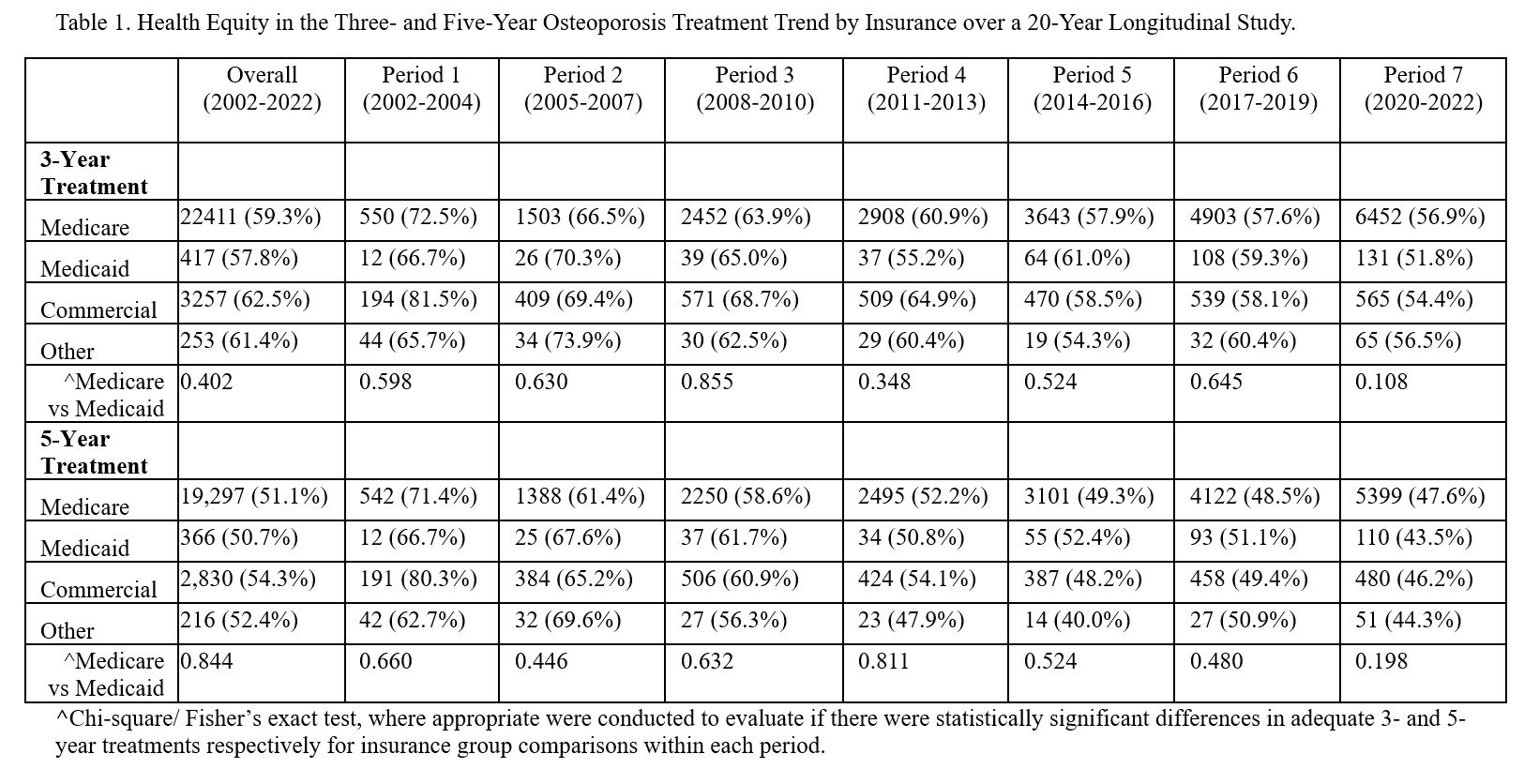
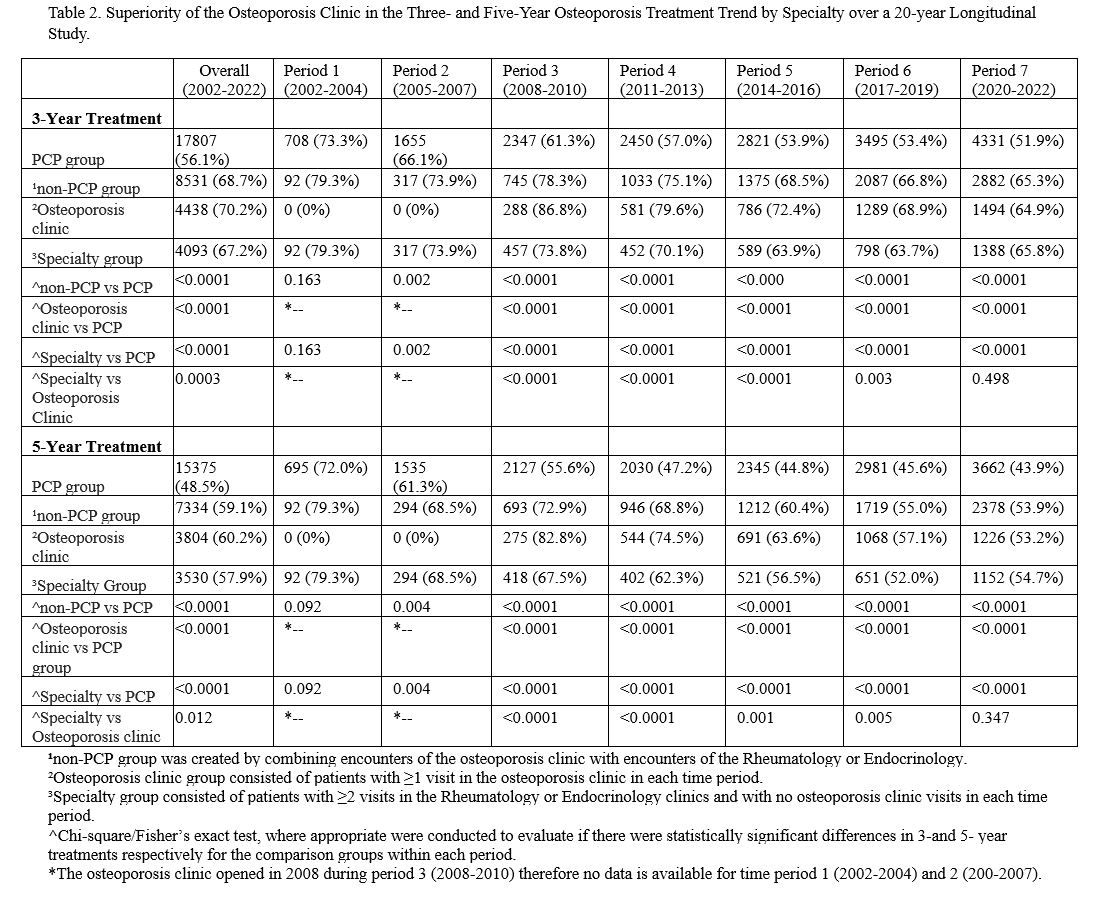
Results: Population included 44,135 patients with median age 76, white (98.1%), women (90.5%), Medicare (85.8%) and PCP managed (71.9%). 3- and 5-year treatment trends declined from period 1 to 7 (73.9 to 56.5%, p< 0.0001), (72.7% to 47.4%, p< 0.0001) respectively coinciding with national decline in osteoporosis treatment rates (Figure 1). Our treatment rate far exceeds a retrospective study of 48,668 patients 60-80 years old with < 20% screening/treatment rates pre-fracture (Ross et al, 2021; doi:10.2106/JBJS.OA.20.00142). Overall treatment was equitable independent of Medicare or Medicaid insurance type for the 3-year (59.3% vs 57.8%, p=0.40) and 5-year (51.1% vs 50.7%, p=0.84) groups with similar pattern in period 1-7 (Table 1). Overall 3- and 5-year treatments with the osteoporosis clinic were superior to the specialty clinic (70.2% vs 67.2%, p=0.0003), (60.2% vs 57.9%, p=0.012) respectively. Similarly, overall 3- and 5-year treatments with the osteoporosis clinic were superior to the PCP alone (70.2% vs 56.1%, p< 0.0001), (60.2% vs 48.5%, p< 0.0001) respectively. This pattern was seen in each period except period 7 where the osteoporosis clinic and specialty group performed similarly during the COVID-19 pandemic (Table 2). The 5-year overall treatment rate was equitable independent of race, but statistically better for women and younger patients (50-64 years old).
Conclusion: This is a unique 20-year study of 3- and 5-year osteoporosis treatment rates (59.7%, 51.5%) with involvement of a focused osteoporosis program for easy identification and treatment of high-risk patients. The osteoporosis clinic care was superior to the PCPs and specialty clinic. Treatment was equitable independent of insurance or race. By using a specialized osteoporosis clinic and a personalized DXA report with embedded diagnosis and treatment recommendations, we created a unique care structure that serves to bridge the osteoporosis care gap and is easily replicable.
To cite this abstract in AMA style:
Chukwu N, Chang L, Olenginski T, Srinivasan H, Udoeyo I, Pugliese D, Berger A, Cote J. Providing Optimal and Equitable Osteoporosis Treatment Using a Programmatic Approach -A 20 Year Longitudinal Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/providing-optimal-and-equitable-osteoporosis-treatment-using-a-programmatic-approach-a-20-year-longitudinal-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/providing-optimal-and-equitable-osteoporosis-treatment-using-a-programmatic-approach-a-20-year-longitudinal-study/