Session Information
Session Type: Abstract Session
Session Time: 1:00PM-2:30PM
Background/Purpose: Social determinants of health (SDoH), including non-medical social needs and adverse environmental exposures, contribute to inequities in rheumatic disease care and outcomes. Patients with rheumatic conditions receive extensive care in the subspecialty setting, where SDoH are infrequently documented and infrastructure to address needs is lacking. We implemented SDoH screening in a multihospital system, offered assistance to help address needs, and examined changes in SDoH needs on a subsequent screen.
Methods: We implemented an electronic health record-based SDoH screening survey for patients with upcoming appointments at 9 rheumatology clinics across 2 hospitals. Patients who indicated SDoH needs received need-specific lists of community resources, and those requesting further information received telephone outreach by a rheumatology-based Community Resource Specialist (CRS) with individually tailored guidance to facilitate access to resources. Patients who indicated “no information needed” received neither. Patients who missed the visit associated with a completed screen, or with a visit following minor modifications in screening procedures by the hospital system, were rescreened. We examined the prevalence of needs between the baseline (“Screen 1”) and subsequent (“Screen 2”) screen, completed ≥30 days apart, and used a Pearson’s chi-squared test to assess for a difference in persistence of ≥1 overall need between assistance groups. A need was considered persistent if it was present in both screens.
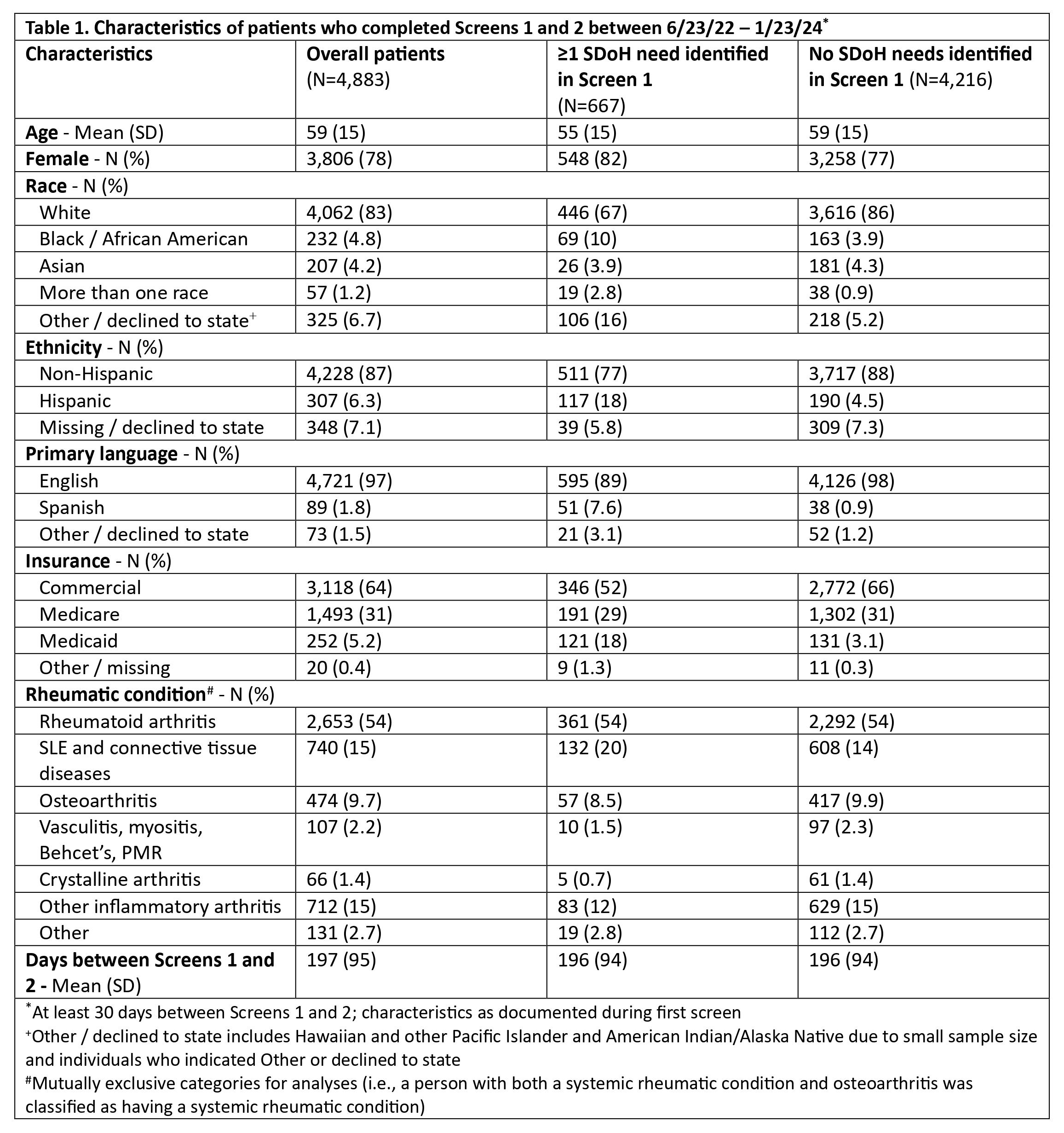
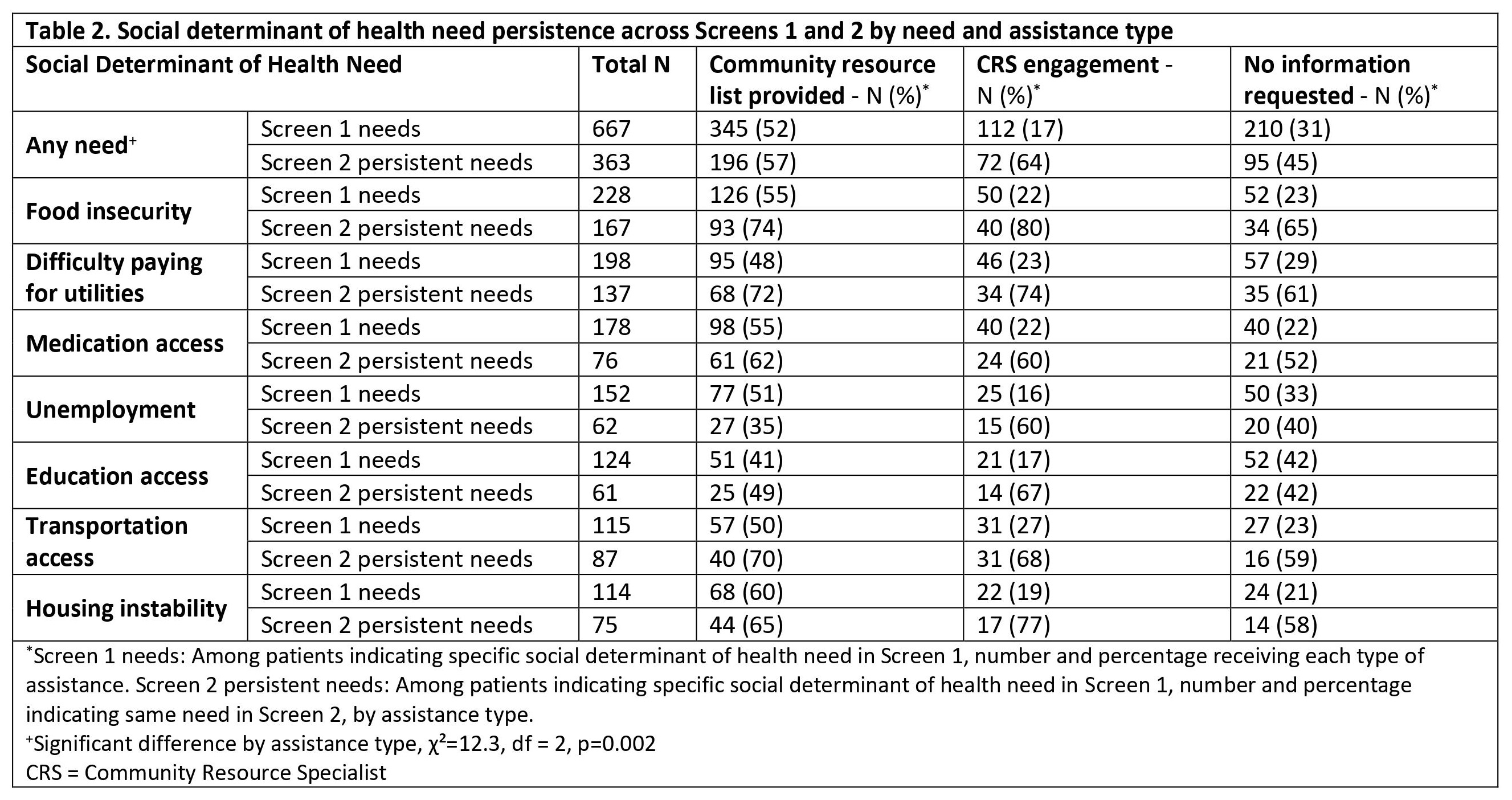
Results: Between 6/23/22-12/23/23, 10,521 adults (≥18 years) completed the rheumatology-based SDoH screening. Of these, 4,883 (46.4%) were rescreened (mean (SD) 196 (94) days between screens) (Table 1). Among those who completed both screens, 667 (14%) had ≥1 need in Screen 1 (mean (SD) 1.7 (1.3) needs). Individuals with (vs. without) needs were younger and a higher percentage were female, identified as Black or Hispanic, and were Spanish-speaking. In Screen 2, 363 (54%) of the 667 patients with ≥1 need on Screen 1 again had ≥1 need (mean (SD) 1.0 (1.3) needs). The most frequent needs in Screen 1 were food insecurity (34%), difficulty paying for utilities (30%), and medication access issues (27%); these needs also persisted across screens, with >50% with remaining needs. Patients requesting no information had the lowest percentages of need persistence. For all needs except medication access, patients who received CRS engagement were more likely to have persistent needs (Table 2).
Conclusion: This program revealed a significant burden of persistent and dynamic SDoH needs, demonstrating the importance of repeated rheumatology-based screening. Patients who received CRS assistance often had persistent needs on rescreen. Possible explanations include the presence of more complex needs, needs rooted in poverty requiring societal-level change and sustained support, and increased patient comfort disclosing their needs after initial CRS interaction. Further studies with random assignment to interventions and longer follow-up are needed to assess the impact of SDoH screening on rheumatic disease inequities.
To cite this abstract in AMA style:
Gim H, Summit R, Retzel K, Santacroce L, Bills V, Shadick N, Schoenfeld S, Feldman C. Changes in Social Determinants of Health Needs Uncovered by a Rheumatology-Based Screening and Assistance Program [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/changes-in-social-determinants-of-health-needs-uncovered-by-a-rheumatology-based-screening-and-assistance-program/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/changes-in-social-determinants-of-health-needs-uncovered-by-a-rheumatology-based-screening-and-assistance-program/