Background/Purpose: Recommended treatment for DMARD naïve patients is methotrexate (MTX) with or without glucocorticoids (GCs). Triple DMARD therapy however is not recommended, because well proven evidence of superior efficacy is suggested to be lacking. Furthermore possible drug toxicities might influence the physician’s choice of induction therapy. Therefore, our aim is to compare one-year clinical efficacy of: (1) triple DMARD therapy vs. MTX mono-therapy and (2) oral GCs bridging therapy vs. 1 dose of intramuscular (im) GCs in patients with early RA.
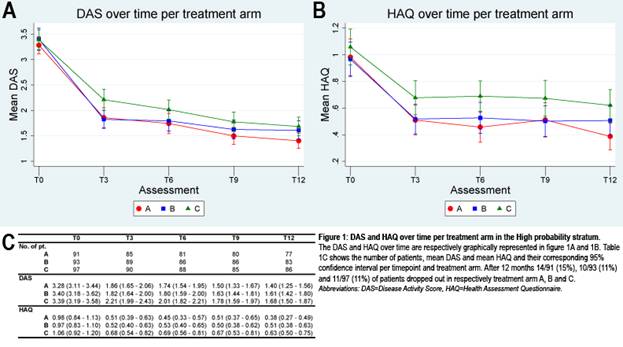
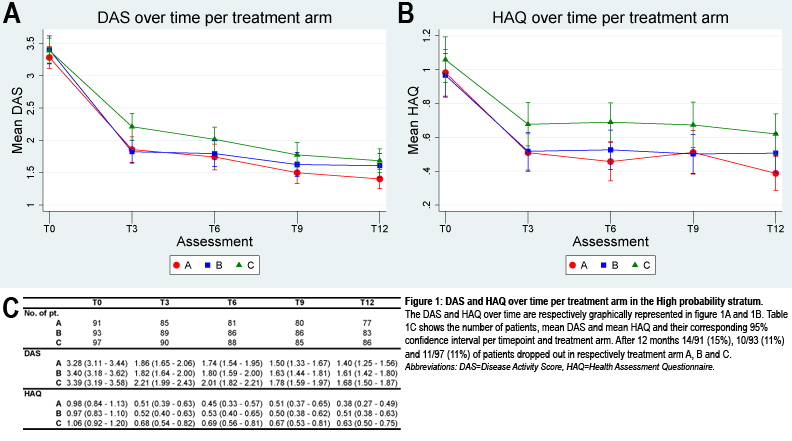
Methods: The one-year data of single-blinded randomized clinical trial in patients with recent-onset arthritis (tREACH) were used. Patients were included who had a high probability (> 70%) of progressing to persistent arthritis, based on the prediction model of Visser. The Visser algorithm and 2010 criteria for RA have similar discriminative abilities to identify patients at risk of persistent arthritis at 1 year. Patients were randomized into 3 induction therapy strategies: (A) triple DMARD therapy (MTX 25 mg + sulfasalazine (SASP) 2 gr. + hydroxychloroquine (HCQ)) 400 mg with im GCs (Depomedrol 120mg), (B) triple DMARD therapy with an oral GCs tapering scheme (starting 15 mg) and (C) MTX with oral GCs similar to B. Treatment strategies were ‘tightly controlled’, with patients being examined every 3 months and treatment decisions based upon the original DAS thresholds for low disease activity. We investigated following response parameters over time: DAS, HAQ, using the area under the curve (AUC). We also looked at radiographic progression after 12 months of therapy, medication usage and adverse events.
Results: A total of 281 patients were included in the high probability stratum and randomly assigned to (A) (n=91), (B) (n=93) or (C) (n=97). Patients were mostly females (68%) with an average symptom duration of 166 days (95% CI: 156 – 177). At baseline 267 (95%) of patients fulfilled the 2010 criteria for RA, 216 (77%) patients were ACPA positive and 48 (16%) patients had erosions. Over time disease activity and functional ability were respectively -2·39 (-4·77 to -0·00, 95%CI) and -1·67 (-3·35 to 0·02, 95%CI) lower in patients with triple DMARD therapy compared with MTX mono-therapy. After 3 months, less treatment failure occurred in the triple DMARD therapy groups, resulting in the prescription of 50% fewer biologicals. This difference remained over time. No differences were seen between both GC bridging therapies. Respectively 15%, 30%, and 18% of patients in arm A, B, and C had radiographic progression after 1 year. No differences in serious adverse events were seen.
Conclusion: In patients with early RA triple DMARD therapy is superior to MTX mono-therapy even after 12 months of therapy. Furthermore both intramuscular and oral GCs can be used as bridging therapy.
Disclosure:
P. H. P. de Jong,
None;
J. M. W. Hazes,
None;
K. H. Han,
None;
A. M. Huisman,
None;
D. van Zeben,
None;
P. A. van der Lubbe,
None;
A. H. Gerards,
None;
B. van Schaeybroeck,
None;
P. B. de Sonnaville,
None;
M. V. Krugten,
None;
J. J. Luime,
None;
A. E. A. M. Weel,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/initial-triple-dmard-therapy-is-more-efficient-than-methotrexate-monotherapy-in-recent-onset-rheumatoid-arthritis-1-year-data-of-a-randomized-clinical-trial-treach/