Session Information
Date: Monday, November 18, 2024
Title: Osteoporosis & Metabolic Bone Disease – Basic & Clinical Science Poster
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Glucocorticoid induced osteoporosis (GIOP) accelerates bone loss and increases fracture risk. We evaluated GIOP screening and prescribing patterns in our Veterans Affairs (VA)-based academic rheumatology clinic. Our quality improvement work focused on 1) prescription of supplemental calcium and vitamin D, 2) dual-energy x-ray absorptiometry (DXA) scan ordering, 3) FRAX risk stratification and assessment of appropriate osteoporosis (OP) medication prescribing including oral or IV bisphosphonate, PTH-analogues, denosumab, or romosozumab.
Methods: Veterans on chronic GC (≥2.5mg prednisone, ≥ 3 months) with an active prescription from a rheumatology provider were extracted in a data pull on 3/14/24. Prescription data for supplemental calcium, vitamin D (Ca/D), and OP medication were also included. GC dose and duration, calcium intake, DXA scans, left femoral-neck T score (LFNTS) were recorded and manually validated, including data through 6/1/24. FRAX scores were calculated for each patient using the University of Sheffield FRAX calculator. FRAX score for major osteoporotic fracture (MOF) and hip fracture risk was increased by 15% and 20% for GC use >7.5mg/day per ACR guidelines. Patients were risk-stratified as very high (LFNTS ≤-3.5 or FRAX 10 yr risk of MOF and hip fracture of ≥30% and ≥4.5% respectively), high (LFNTS ≤-2.5 or FRAX 10 yr risk of MOF and hip fracture of ≥20% and ≥3% respectively), moderate (FRAX 10 yr risk of MOF and hip fracture of 10-20% and 1-3% respectively) or low risk (FRAX 10 yr risk of MOF and hip OP fracture of < 10% and < 1% respectively). For patients without recent DXA, clinical FRAX data were calculated without BMD. We recorded rates of Ca/D prescription, DXA test completion, and OP medication utilization based on FRAX risk category.
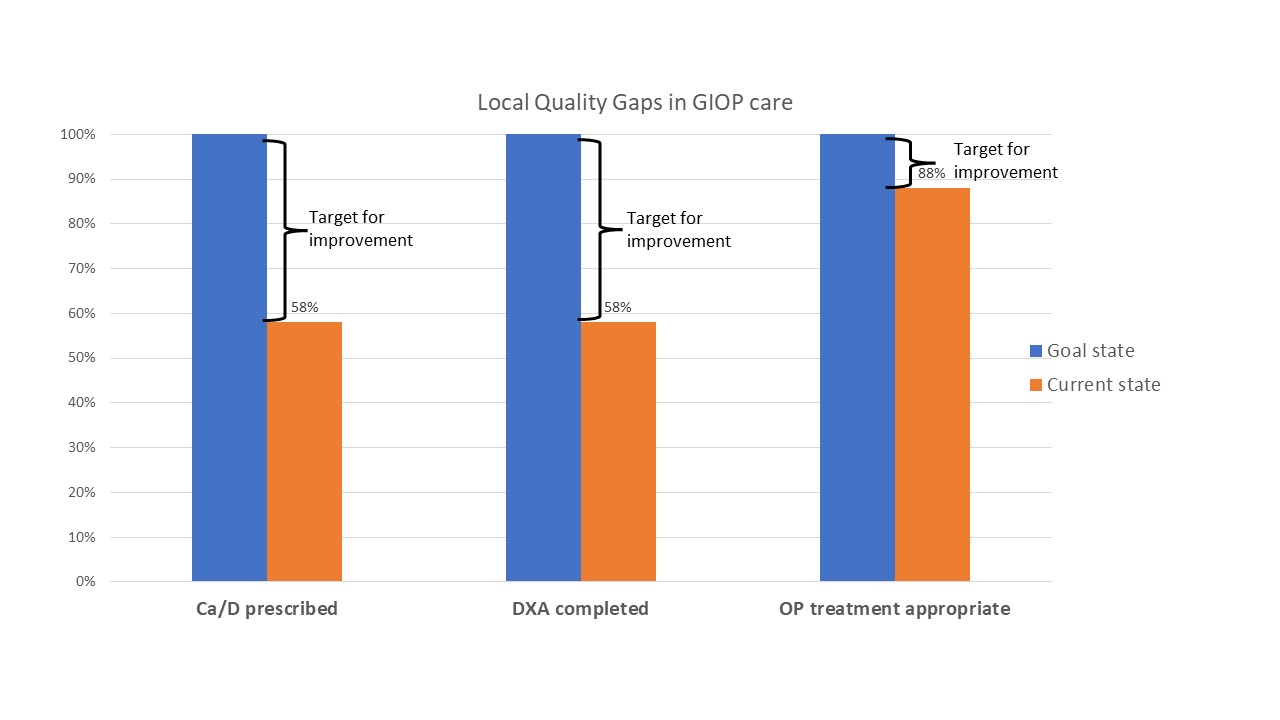
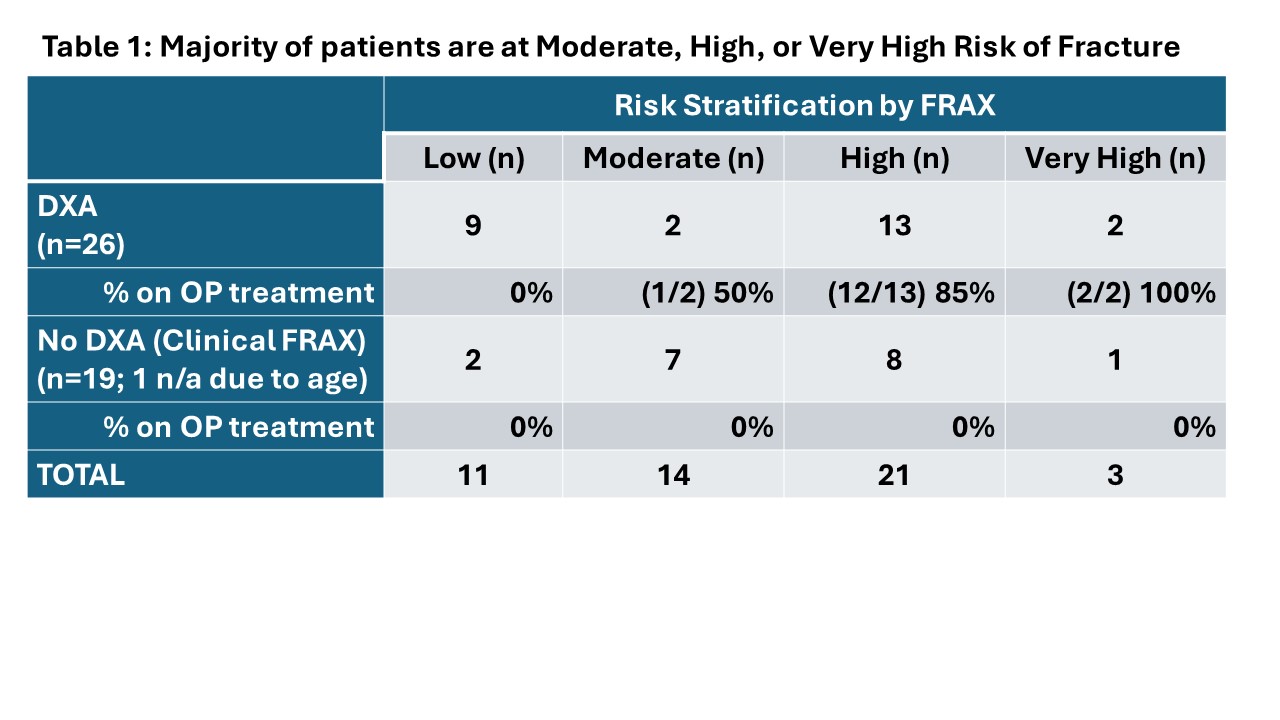
Results: Forty-five patients were included in the data pull. Of 45, twenty-six (58%) were prescribed Ca/D. Twenty-six (58%) had DXA within 2 years and 19 (42%) did not. Of those with a recent DXA, FRAX calculations resulted in classifying 2 patients as very high risk, 13 as high risk, 2 as moderate risk, and 9 as low risk. Of the 17 moderate to very high-risk patients, 15 (88%) were on OP therapy; of the two who were not, one had an expired prescription and one declined treatment. Of the 19 patients without recent DXA, 10 had never had DXA, 3 had testing >5 years prior, and 4 were on GC without updated imaging. Clinical FRAX was calculated in patients without DXA (except 1 who was < 40 years). Of these, one was very high risk, 8 (42%) were high risk, 7 (36%) were moderate risk, and two were low risk; none were on OP therapy.
Conclusion: In our VA-based academic rheumatology practice, veterans on chronic GC do not consistently receive Ca/D supplementation and are under-screened according to the 2022 GIOP guideline, though patients with DXA testing are appropriately treated. Clinical FRAX should be considered in patients without recent DXA. Developing population health tools to improve monitoring in this population remains challenging as many data domains in GIOP care require chart validation (true GC use vs. taper, over-the-counter calcium use, risk factors, DXA results) or calculation (FRAX).
To cite this abstract in AMA style:
Bahia J, Steppe C, Brubeck H, Narla R, Mount G, Wahl E, Wysham K. Rheum for Improvement: Screening and Treatment of Glucocorticoid Induced Osteoporosis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/rheum-for-improvement-screening-and-treatment-of-glucocorticoid-induced-osteoporosis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheum-for-improvement-screening-and-treatment-of-glucocorticoid-induced-osteoporosis/