Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Up to 70% of the 236 million people who have been diagnosed with COVID-19 develop some post-COVID symptoms, i.e. post-acute sequalae of SARS-CoV-2 (PASC) or Long COVID.(1) Long-COVID causes significant physical and mental limitations,(2) including multiple symptoms and organ involvement, even two years after infection.(3) We and others have reported autonomic nervous system (ANS) dysfunction as a contributor to these complaints.(3,4,5) This abstract follows up our ACR2022 report (4) on the importance of medical grade heart rate variability (HRV) as a valuable diagnostic tool in confirming ANS dysfunction in Long- COVID patients. The primary objective of this study was to report an ongoing evaluation of patients with Long-COVID, with symptoms of multiple diversity, and to confirm the value of measuring medical grade HRV, and consider attribution of symptoms to dysautonomia.
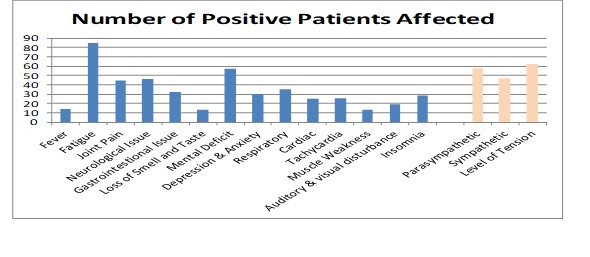
Methods: Patients with Long-COVID (definitive diagnostic evidence and symptoms for post COVID for at least 3 months) were evaluated in a single COVID clinic in Florida. These patients displayed multiple symptoms (Table 1). ANS function in all patients was measured by 5-min, supine HRV (Inmedix, Normandy Park, WA, USA ). Standard 1996 time-and frequency-domain and 2002 Bayevsky (6) HRV indices were assessed (Omegawave Oy, Espoo, Finland).
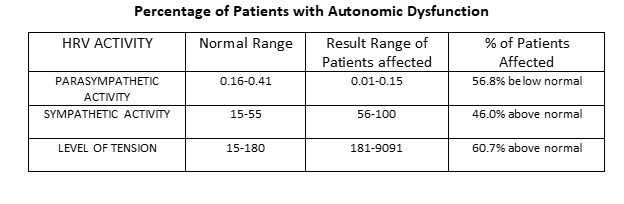
Results: A majority (62.7%) of 102 patients with Long COVID tested (mean age:43 yrs; mean duration:15 mo.) showed findings of dysautonomia by abnormal resting HRV. (Table 2) Of the 62.7% patients with clinical findings of ANS dysfunction, 90.6% had low parasympathetic activity, 73% had increased sympathetic activity and 98.4% had increased levels of tension. Significant symptoms of dysautonomia were fatigue (83.3%), dyscognition (55.8%), neurological (45%), gastrointestinal (31.3%), cardiac (24.5%) and depression or anxiety (29.4%). (Table 2)
Conclusion: Long COVID or post-acute sequalae of SARS-CoV-2 (PASC) patients, are often evaluated by rheumatologists. We have confirmed that ANS dysregulation documented by medical grade HRV was prominent among this patient population. Others have reported the interplay between the ANS and inflammation across systemic autoimmune disorders (7,8,9). Utilizing the abnormal HRV findings – whether increased sympathetic findings, decreased parasympathetic findings or both – may reveal an opportunity to address ANS imbalance and subsequently ameliorate this morbidity.
Further exploration of ANS abnormalities and application of medical-grade HRV in Long COVID is warranted.
REFERENCES
1. Lancet Respir Med. 20219(11):1275-1287.
2. Center for Disease Control (CDC) 2023;72(32);866-870.
3. Fernandez-de-las-Penas et al. J Infect. 2024;88(2);77-88.
4. Gaylis, et al. Arthritis Rheumatol. 2022; 74 (suppl 9).
5. Dani, M et al. ClinMed 2020-0896.
6. Bayevsky RM, , et al. HRV Analysis under the usage of different electrocardiography systems prepared according to the order of the Committee of Clinic Diagnostic Apparatus and the Committee of New Medical Techniques of Ministry of Health of Russia (protocol №4 from the 11APR2002).
7. Sharma, C. Nature Reviews Rheumatology 2023;19, 399-404.
To cite this abstract in AMA style:
Gaylis N, DeLaRosa O, Sagliani J, Holman A. Autonomic Nervous System Dysfunction Common Among Patients with Long COVID:Diagnosis and Treatment Implications [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/autonomic-nervous-system-dysfunction-common-among-patients-with-long-coviddiagnosis-and-treatment-implications/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/autonomic-nervous-system-dysfunction-common-among-patients-with-long-coviddiagnosis-and-treatment-implications/