Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: Although rheumatoid arthritis (RA) increases cardiovascular disease (CVD) risk, RA patients receive less CVD preventive care than peers. We previously showed gaps in lipid testing and hypertension diagnosis despite more clinic visits in RA patients compared to peers. This qualitative study aimed to examine the processes by which RA patients experience CVD preventive care in order to inform patient-centered interventions to close these gaps.
Methods: Ten adult RA patients were recruited from 3 local rheumatology clinics for interviews to evaluate CVD preventive care experiences beyond clinical documentation. Interviews were recorded, transcribed, dual coded and team reviewed using NVivo software to facilitate grounded theory analysis and interpretation (Strauss 1994).
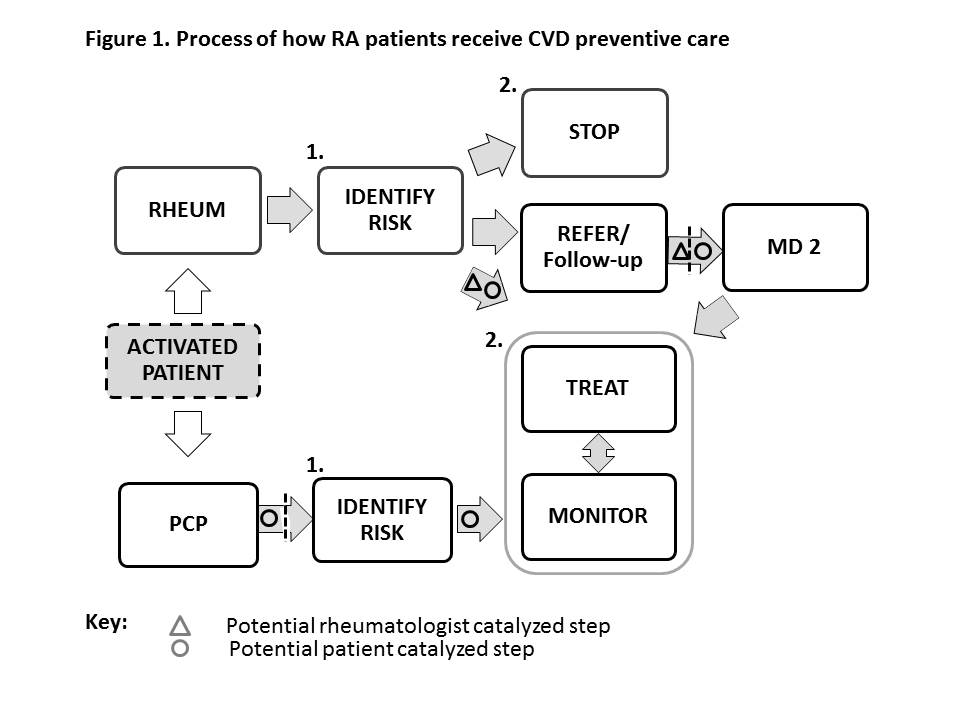
Results: Interviewed RA patients were 70% female, ages 23-81 (mean 57). Most RA patients were unaware of increased CVD risk while all patients were aware of RA medication side effects. Those who had experienced CVD risk management described two processes by which they received CVD preventative care: 1) identifying risk and 2) action (Figure 1). The number of steps and likelihood of actions were related to the physician who identified risk. Primary care physicians were not specifically described as identifying RA-CVD risk, but if they identified traditional CVD risks were most likely to actively manage them. However, many patients described rarely seeing their PCP, which is consistent with national reports. Rheumatologists more often identified RA-specific risk, but rarely provided active CVD risk treatment or monitoring. Therefore, a particularly concerning finding was that 60% of participants perceived their rheumatologist as their main provider, since the reliance on this provider may delay or decrease treatment likelihood. A few participants alternatively described steps in which they themselves identified RA-specific risk and self-advocated care (Fig 1. O’s). Overall, most patients had no preference about who managed CVD risks, expecting that blood pressure or cholesterol would be addressed. Future work should examine actual rheumatologist and PCP CVD risk identification and actions, and provider perceptions to inform future interventions. Optimizing roles may include RA patient activation (O) and rheumatologist communication/co-management (D) to catalyze CVD risk identification and management.
Conclusion: Patients with RA do not report receiving consistent CVD preventive care. Most described their rheumatologist as their main doctor and noted infrequent PCP visits, though rheumatologists were less likely than PCP’s to actively manage CVD risks. This suggests that RA patient activation, rheumatologist communication/co-management and advocating regular PCP care should be studied as potential interventions to close CVD-preventive care gaps in RA.
Disclosure:
C. M. Bartels,
None;
S. Tweddell,
None;
B. Bowers,
None;
E. Jacobs,
None;
T. Roberts,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/rheumatoid-arthritis-patient-cardiovascular-disease-prevention-experiences-qualitative-analysis-and-implications/