Session Information
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Sarcoidosis is a condition affecting multiple organ systems, characterized by the presence of non-caseating granulomas. Cardiac sarcoidosis (CS) is a challenging diagnosis, with a prevalence of 5% to 10% among sarcoidosis patients, varying significantly across studies. Small-scale studies have shown differences in CS prevalence and presentation between Caucasians and African American (AA) individuals. However, comprehensive real-world data from a large national cohort is lacking. This study addresses this gap in understanding cardiac sarcoidosis.
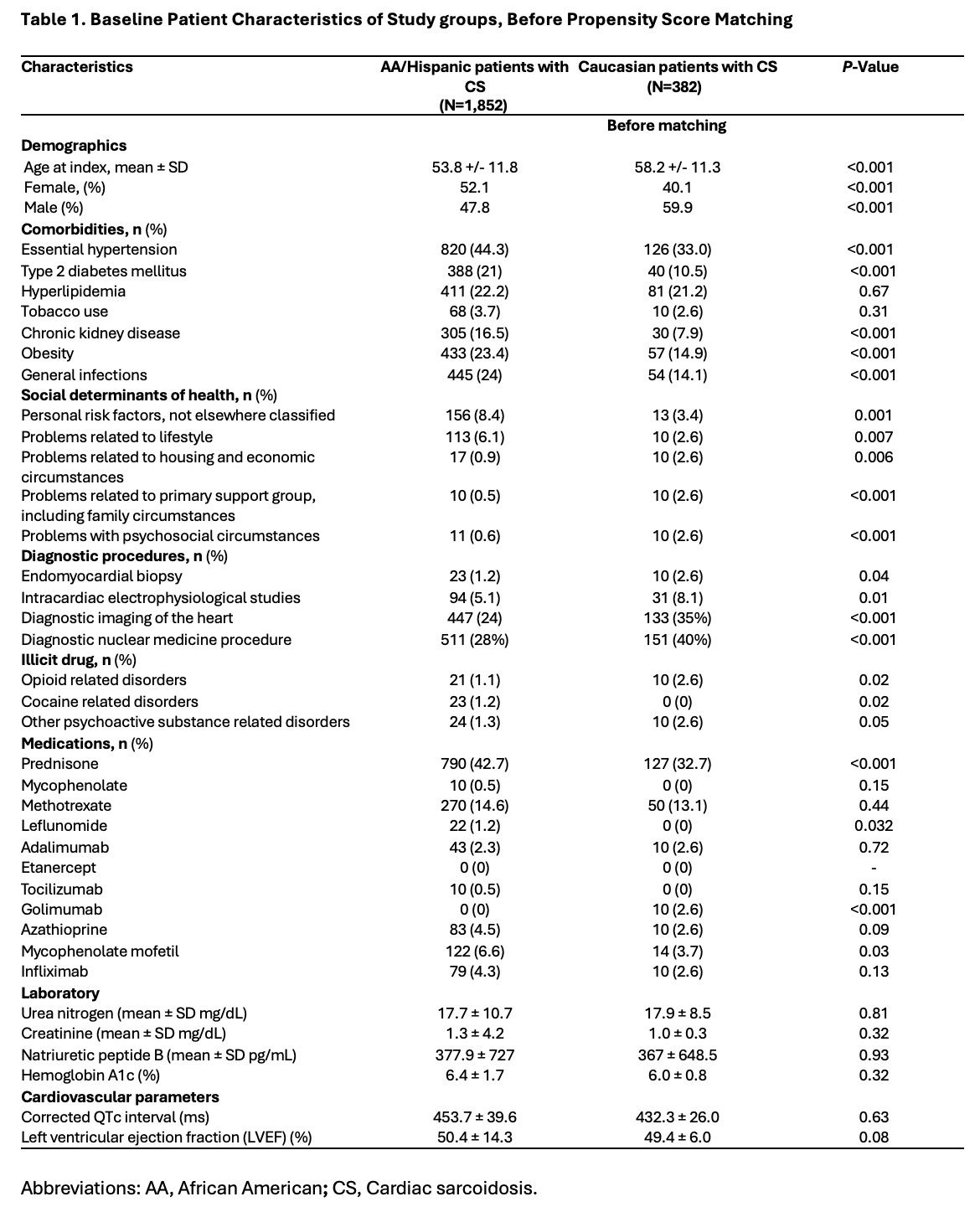
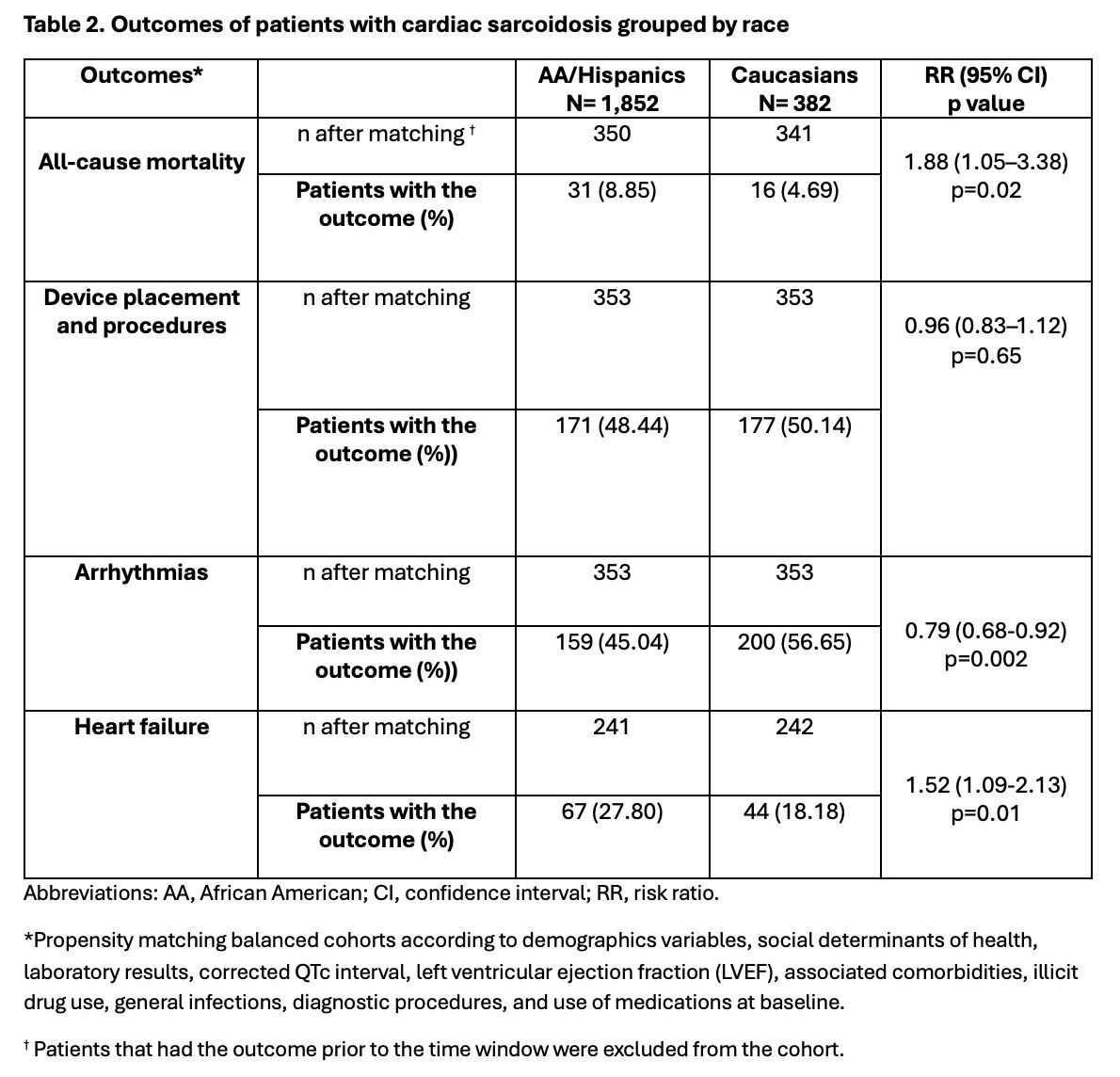
Methods: This is a nationwide, retrospective study. We used the global, multicenter research network (TriNetX) database from 88 large healthcare organizations across multiple countries. We included patients over 18 years with CS diagnosed between January 1, 2014, and June 8, 2024, using ICD-10 and ICD-9 codes. Patients were compared based on race (Caucasians vs. Hispanic or Latino and AA) using 1:1 propensity score matching. Matching accounted for demographics (age at diagnosis and gender), social determinants of health, laboratory results, QTc interval, left ventricular ejection fraction (LVEF), chronic associated comorbidities, illicit drug use, infections, diagnostic procedures, and medication use at baseline. Outcomes included all-cause mortality, device implantation, heart failure and arrhythmias. Exposure for outcomes was anytime post-index diagnosis, excluding patients with pre-index event outcomes, endocarditis, or ischemic heart disease. Risks ratios (RR) with 95% confidence intervals were calculated for each outcome, with a p-value < 0.05 considered significant.
Results: We identified 1,852 Hispanic/AA and 382 Caucasian CS patients. Mean age at diagnosis was 53.8 ± 11.8 and 58.2 ± 11.3 years for AA/Hispanic and Caucasian patients, respectively. Caucasians were more often males (59.9%), while AA/Hispanics were more often females (52.1%). Comorbidities (hypertension, type 2 diabetes, chronic kidney disease, and obesity), cocaine use, elevated HgA1C, and infections were more common in AA/Hispanics. Caucasians underwent more diagnostic studies (including endomyocardial biopsy and cardiac imaging) and had higher opioid use and more negative social determinants of health at baseline. After matching, AA/Hispanic patients had higher all-cause mortality risk (RR=1.88, CI95% 1.05, 3.38; p=0.02) and heart failure (RR= 1.52, CI95% 1.09,2.13; p=0.01) but lower risk of arrhythmias (RR=0.79, CI95% 0.68,0.92; p=0.002) compared to Caucasians. No significant difference was found in device implantation rates.
Conclusion: AA/Hispanic patients with CS exhibit higher rates of chronic comorbidities, cocaine use, elevated HgA1C, and infections compared to Caucasians but have a lower risk of rhythm disturbances. Caucasians undergo more diagnostic studies and have higher opioid use and more adverse social determinants of health. Further research is needed to understand disparities in health outcomes and healthcare experiences between these groups.
To cite this abstract in AMA style:
Gonzalez Moret Y, Lema D, Lo k, Rodriguez Quinonez F. Healthcare Disparities and Clinical Outcomes in Cardiac Sarcoidosis. a Retrospective Cohort Study [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/healthcare-disparities-and-clinical-outcomes-in-cardiac-sarcoidosis-a-retrospective-cohort-study/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/healthcare-disparities-and-clinical-outcomes-in-cardiac-sarcoidosis-a-retrospective-cohort-study/