Session Information
Date: Sunday, November 17, 2024
Title: Vasculitis – Non-ANCA-Associated & Related Disorders Poster II
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Polymyalgia rheumatica (PMR) and giant cell arteritis (GCA) are closely related conditions that often co-occur.1 Approximately half of all patients with GCA experience PMR symptoms. On the other hand, the incidence of GCA among patients with PMR varies widely, with estimates ranging from 5 to 30 percent depending on the study.2 PMR may manifest before, alongside, or after the onset of GCA.3,4 We conducted a retrospective analysis of PMR patients at an academic center, focusing on those with concurrent GCA, to identify potential predictors of GCA among PMR patients.
Methods: The study was conducted retrospectively, using data from a rheumatology clinic at an academic medical center. We specifically included patients with a primary diagnosis of provider-diagnosed PMR or PMR associated with Giant cell arteritis (GCA) and a minimum of one year of follow-up. To ensure the study’s focus, we excluded patients with other rheumatological disorders, including GCA, without the features of PMR. 376 PMR patients from 2011 to 2021 met these inclusion criteria, forming the basis of our analysis.
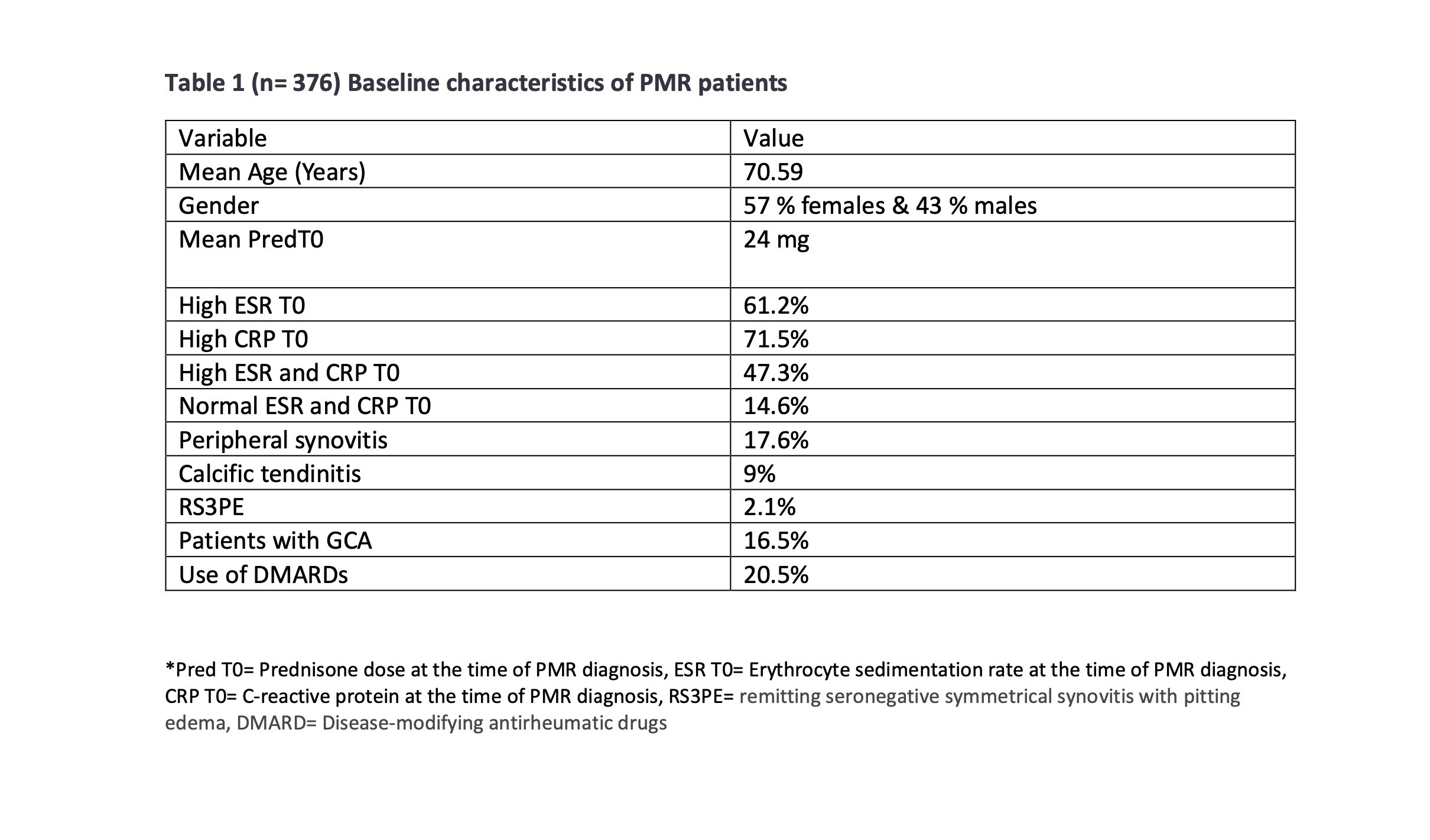
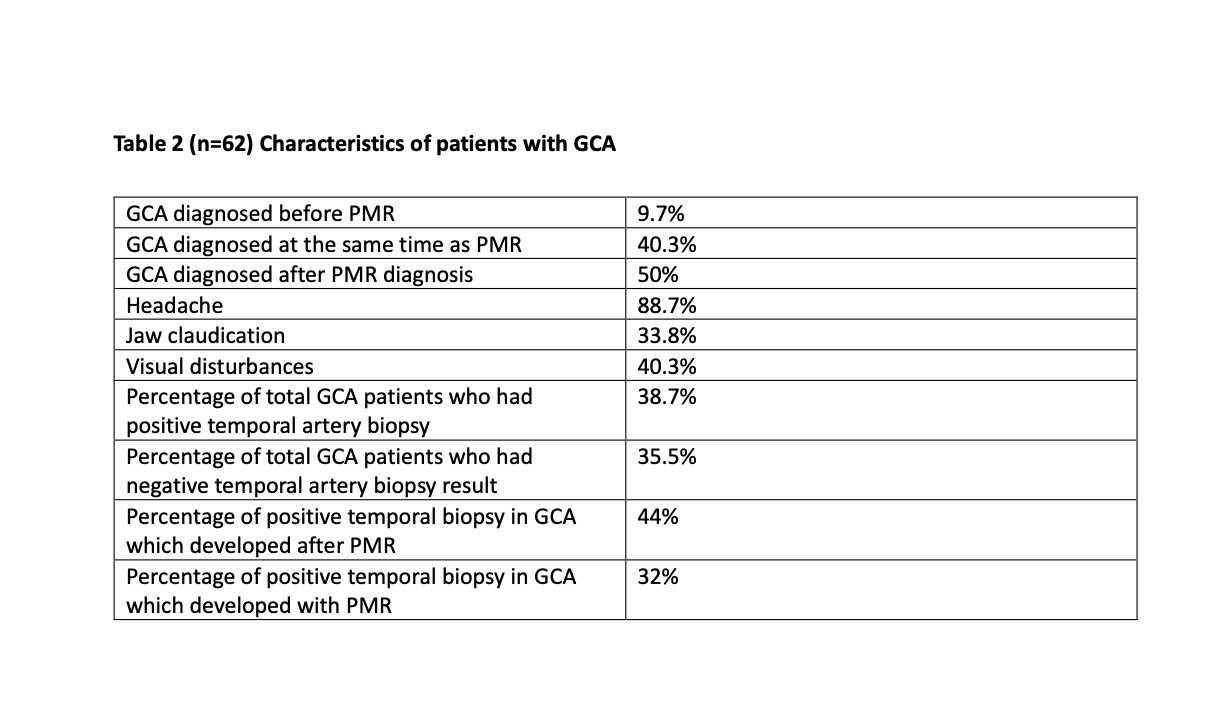
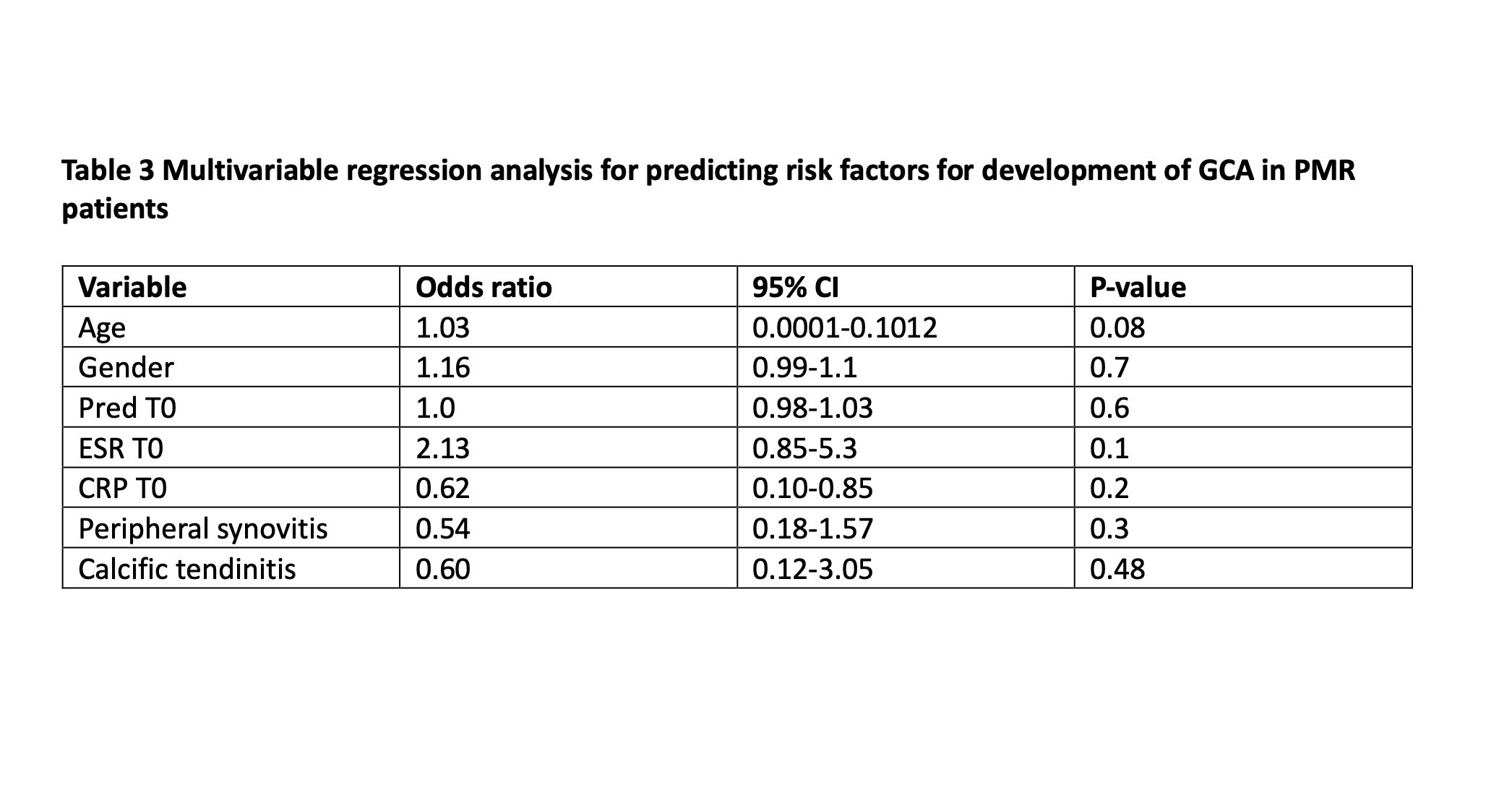
Results: The mean age of the patient population was 71 years, with 57 % being females and 43 % males. (Table 1). Among the 376 PMR patients, 16.5% had a concurrent diagnosis of GCA, which usually developed alongside (40.3%) or after the PMR diagnosis (51%). Headache, jaw claudication, and visual disturbances were the most common symptoms reported. 74.2% of the GCA patients had bilateral temporal artery biopsy done, and 44% of the GCA patients who presented with PMR had positive arteritis on pathology. The percentage of positive temporal artery biopsy was still 32% in the patients who developed GCA after PMR diagnosis. (Table 2). 17.5 % of all the PMR patients had features of peripheral synovitis, 9 % had calcific tendinitis on hip and shoulder X-rays, and approximately 2% of total patients presented with RS3PE (remitting seronegative symmetrical synovitis with pitting edema). A majority of patients exhibited elevated markers of inflammation (ESR or CRP), with only 14.6% presenting with normal values initially. A multivariable logistic regression analysis assessed potential predictive factors associated with developing GCA in PMR patients. Still, no baseline characteristic had a statistically significant association. (Table 3)
Conclusion: The study’s findings are significant, revealing that 16.5% of PMR patients also had GCA, often developing it concurrently or following the PMR diagnosis. Even in PMR patients who developed GCA later in the disease course and after steroid treatment, temporal artery biopsy positivity remained at 32%. Despite extensive analysis, no baseline characteristic emerged as a statistically significant predictor for the development of GCA among PMR patients. These findings underscore the need for ongoing clinical vigilance and further research to identify reliable predictors to enhance these patients’ management and treatment strategies. It’s important to note the study’s limitations, including its retrospective nature and relatively small sample size of the GCA patients, which might have interfered with ascertaining the predictive factors associated with developing GCA in PMR patients.
To cite this abstract in AMA style:
Tiwari V, fang c, Campbell E, loomba K, Khubchandani N, shah s, Rigby W. Co-occurrence of Giant Cell Arteritis and Polymyalgia Rheumatica: Insights from a Retrospective Analysis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/co-occurrence-of-giant-cell-arteritis-and-polymyalgia-rheumatica-insights-from-a-retrospective-analysis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/co-occurrence-of-giant-cell-arteritis-and-polymyalgia-rheumatica-insights-from-a-retrospective-analysis/