Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: The idiopathic inflammatory myopathies (IIM) are associated with interstitial lung disease (ILD), characterized by parenchymal abnormalities on high-resolution computed tomography (HRCT). We determined the radiologic progression of IIM patients with ILD using a novel lung parenchymal scoring system, “Computer-Aided Lung Informatics for Pathology Evaluation and Rating” (CALIPER) software to record abnormalities on HRCT.
Methods: We conducted a retrospective study of dermatomyositis (DM) and polymyositis (PM) patients at a large academic institution in 2003-2011. We collected HRCT and PFT data at IIM diagnosis and 1, 3, and 5 years. HRCT images were anatomically scored using CALIPER: total volume of normal parenchyma, low attenuation areas (mild, moderate, and severe subclasses) and interstitial abnormalities (ground glass opacities, honeycombing, and reticular densities). Definition of improvement (DOI) for ILD was a ≥ 10% increase in total lung capacity (TLC), ≥ 15% increase in diffusing capacity (DLCO), and normalization of oxygen during exercise between baseline and 1 year. Spearman correlations, two group and paired t-tests were performed.
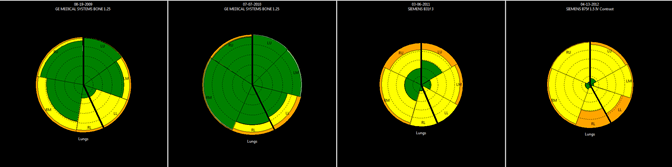
Results: We identified 172 patients with IIM and ILD (62% female; mean age 51 years; mean follow-up 4.1 years). Of those, 59 had DM, 84 had PM, 22 had anti-synthetase syndrome, and 7 were unknown. HRCT images revealed ILD in 95% of patients. Main ILD types were nonspecific interstitial pneumonia (59%), cryptogenic organizing pneumonia (23%), and usual interstitial pneumonia (9%). At year 1, improvement occurred in HRCT scans (n = 58) in percentage of reticular densities from 7 ± 6% to 5 ± 6% (p < 0.001) and interstitial abnormalities from 20 ± 16% to 17 ± 16% (p = 0.049), and a trend in improvement in DLCO (n = 80) from 56.2 ± 18.1 to 58.8 ± 16.6 percent predicted (p = 0.053). Baseline to year 3, improvement occurred (n = 34) in reticular densities (p = 0.011) but no difference in PFT values (n = 64). At year 1, 22 patients met DOI; within these, there was improvement in DLCO (n = 22): 46.8 ± 10.8 to 62.5 ± 12.8 (p <0.001) and TLC (n = 12): 65.9 ± 15.4 to 73.9 ± 13.4 (p = 0.004). Subgroup analysis by treatment, prednisone (group 1; n = 43), prednisone + other immunosuppressant (group 2; n = 65), other immunosuppressant (group 3; n = 18), and none (group 4; n = 40) revealed no differences in PFTs at baseline; but, in group 4 there were more interstitial abnormalities at baseline (p = 0.050). Baseline to year 3, group 4 worsened in interstitial abnormalities (p = 0.036). Progression from normal lung (green) to ground glass opacities (yellow) and reticular fibrosis (orange) also occurred despite treatment (See Figure).
Conclusion: IIM patients with ILD improve in reticular densities, low attenuation areas, and interstitial abnormalities. Progression of ILD was observed in patients without treatment. CALIPER aids in tracking ILD over time.
Figure. CALIPER in ILD.
Disclosure:
K. Wilton,
None;
B. Bartholmai,
None;
S. Kalra,
None;
C. S. Crowson,
None;
H. Khun,
None;
F. C. Ernste,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/use-of-computer-aided-lung-informatics-for-pathology-evaluation-and-rating-software-in-high-resolution-computed-tomography-in-patients-with-idiopathic-inflammatory-myopathy-and-inter/