Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic lupus erythematosus (SLE) is a chronic autoimmune disease with substantial morbidity, particularly in childhood-onset SLE (cSLE). Mental health conditions such as depression and anxiety are common comorbidities in cSLE patients, although less is known about emotional trauma. Glucocorticoids, pivotal in SLE treatment, influence mental health via hypothalamic-pituitary axis regulation, potentially modulating stress responses and psychopathology risk. This study investigates the prevalence of traumatic events, frequency and risk for PTSD symptoms, and their association with demographic and disease characteristics and with depression and anxiety symptoms in a multi-ethnic cohort of cSLE patients.
Methods: We conducted a cross-sectional secondary analysis of prospectively collected data from cSLE patients aged 8-17, diagnosed before 18 years old, meeting ACR 1997 or SLICC classification criteria. Psychiatric assessments used the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL) to assess exposure to 13 types of emotionally traumatic events and to screen for PTSD, depression, and anxiety. Sociodemographic and clinical data were collected through medical chart reviews. Univariate and multivariable logistic regression models were used to examine associations between PTSD symptoms and i) demographic and disease characteristics, ii) depression symptoms, and iii) anxiety symptoms. Multivariable models were adjusted for sex, area-level material deprivation, age at cSLE diagnosis, disease duration, adjusted mean SLEDAI score (over 2 years prior to assessment), and cumulative glucocorticoid dose. We tested for an a priori interaction between PTSD symptoms and glucocorticoid exposure in the depression and anxiety models.
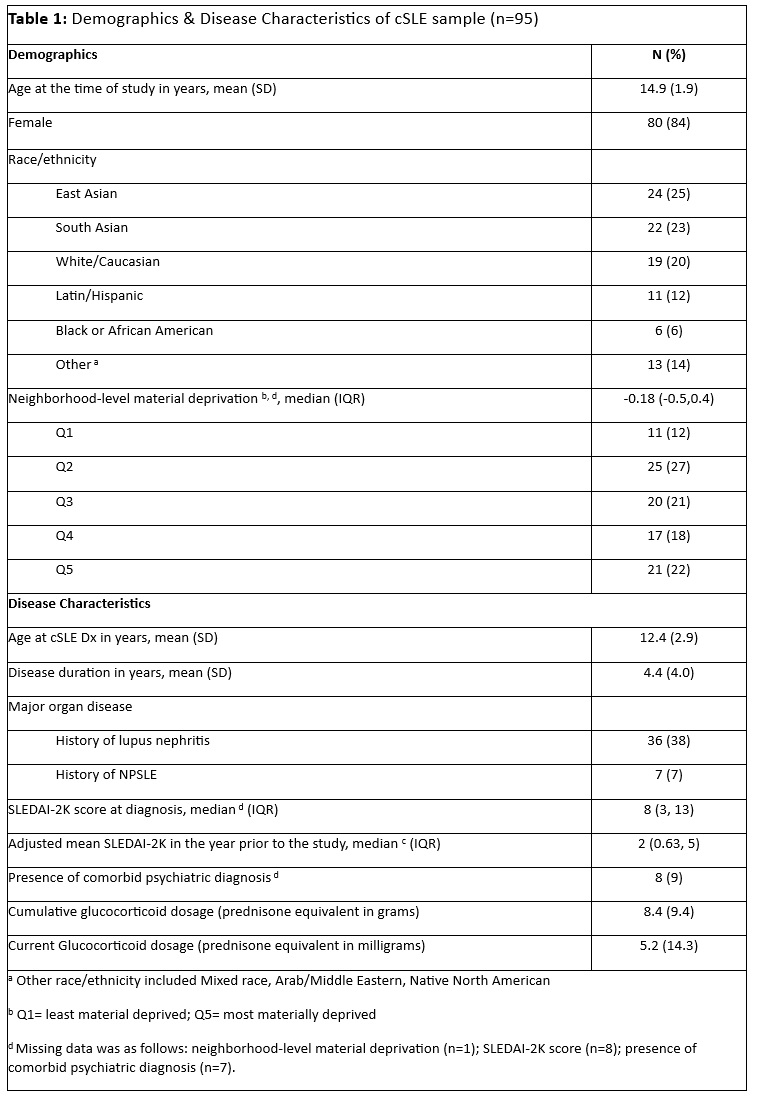
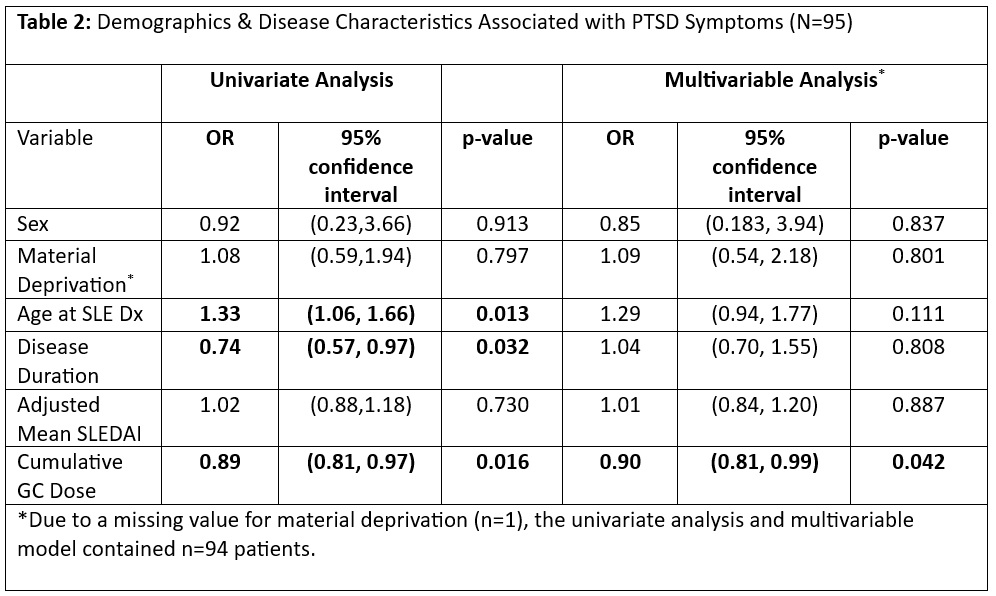
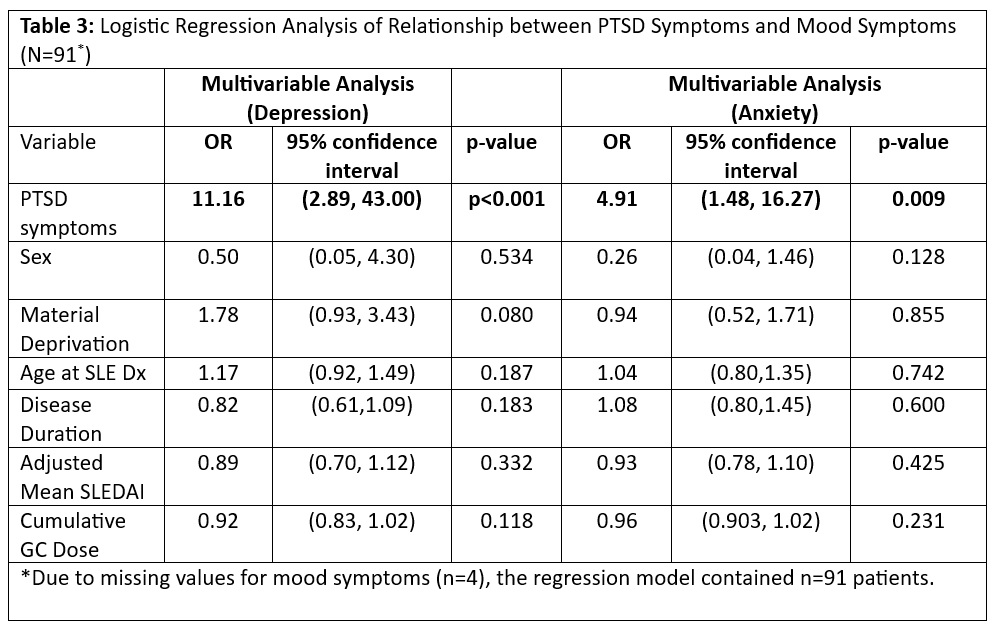
Results: The cohort included 95 cSLE patients (mean age 14.9 years, 84% female) (Table 1). Trauma exposure was reported by 41%, most commonly receiving traumatic news (24%, e.g. family death), witnessing domestic violence (12%), experiencing a car accident (5%), witnessing a disaster (5%), experiencing physical (5%) and sexual (5%) abuse. Symptoms of PTSD were present in 21%, depression in 13%, and anxiety in 35%. In adjusted models, the presence of PTSD symptoms was significantly associated with older age at SLE diagnosis (OR=1.33, 95% CI [1.06-1.66], p=0.013) and lower cumulative glucocorticoid use (OR=0.89, 95% CI [0.81-0.97], p=0.016) (Table 2). PTSD symptoms were significantly associated with depression (OR=15.12, 95% CI [2.66-85.75], p=0.002) and anxiety (OR=4.91, 95% CI [1.48-16.27], p=0.009) after adjusting for covariates (Table 3). The interaction between PTSD symptoms and glucocorticoid was not significant.
Conclusion: Traumatic event history and PTSD symptoms were prevalent in this cSLE cohort. PTSD symptoms were associated with lower cumulative glucocorticoid exposure, but not disease activity, which suggests a potential protective role. Given the strong association of PTSD symptoms with depression and anxiety symptoms, further research is needed to understand the role of PTSD screening and intervention to improve mental health outcomes in cSLE patients.
To cite this abstract in AMA style:
Moaf P, Danguecan A, Quilter M, Couture J, Dominguez D, Ng L, Jeyanathan A, Schachter R, Korczak D, Levy D, Hiraki L, Knight A. An Investigation of Traumatic Events and Mental Health in cSLE [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/an-investigation-of-traumatic-events-and-mental-health-in-csle/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/an-investigation-of-traumatic-events-and-mental-health-in-csle/