Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Systemic Lupus Erythematosus (SLE) disproportionally affects minoritized populations. SLE damage, assessed by SLICC/ACR Damage Index (SDI), is higher in Black than in White US patients, with worse outcomes also in low socioeconomic status. Few studies have investigated how neighborhood disadvantage correlates with outcomes, and how significance of damage varies by organ involvement. We assessed the relationships between race, ethnicity and neighborhood disadvantage on any SDI damage or severe organ damage. We hypothesized that patients in marginalized groups have higher total and severe end-organ damage than non-marginalized peers.
Methods: This observational cohort study included adult prevalent SLE patients from three healthcare systems across one state 1/1/2014-12/31/2020. Abstractors manually validated SLE cases using 1997 American College of Rheumatology (ACR) or 2012 SLE International Collaborating Clinics (SLICC) criteria. Sociodemographics, disease duration, and organ damage were abstracted. SDI was used to assess baseline damage and outcomes through end of study (12/31/2020) or death. Damage events were categorized as severe (cardiac, renal, pulmonary, malignancy or death) or non-severe (other SDI events, e.g., cataract). Neighborhood disadvantage was assessed by area deprivation index (ADI) quintile. Participants were stratified by demographic categories to compare new damage events. Multivariable Cox models assessed hazards ratios (HR, (95% CI)) of new events and new severe events.
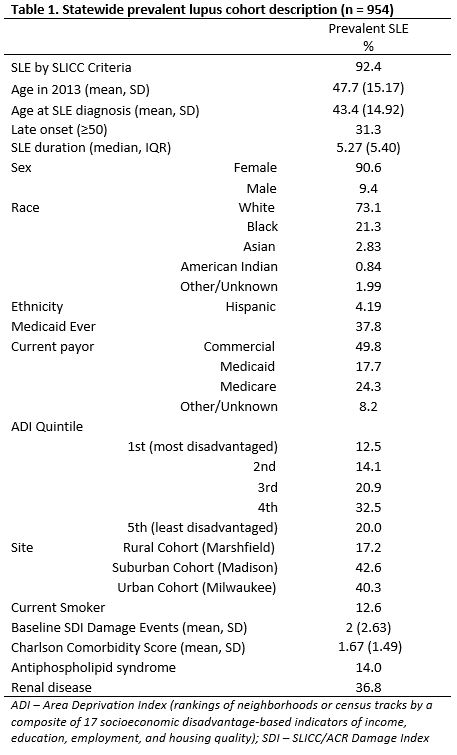
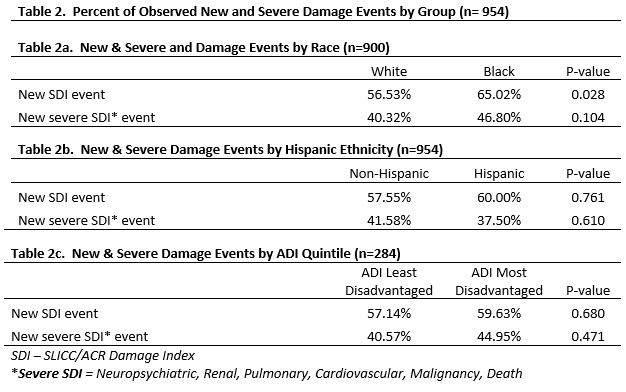
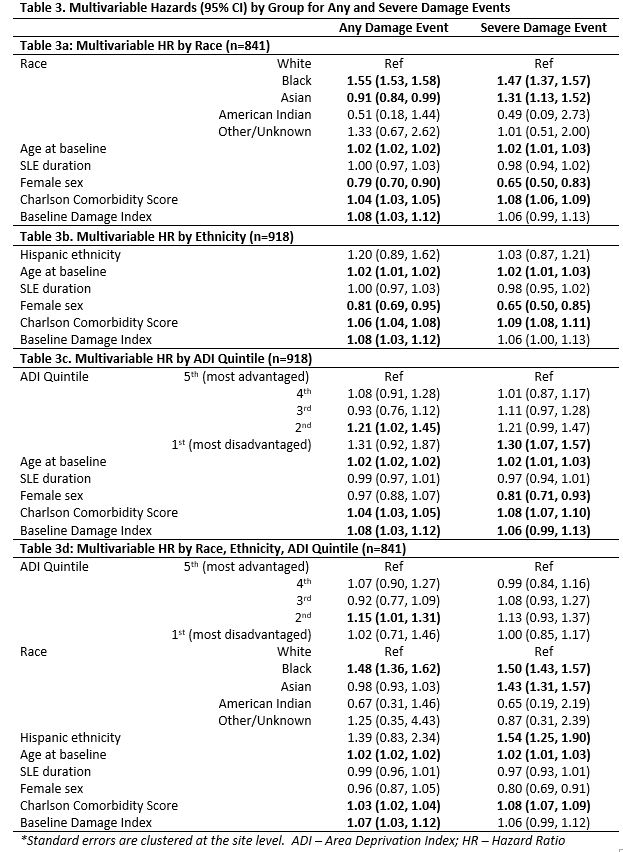
Results: Among 954 patients with SLE, average age was 48, with 91% female and 73% White (Table 1). Black patients showed a higher percentage of new damage events (65% vs. White 57%); no raw differences observed by ADI or Hispanic ethnicity (Table 2). Median observation time was 2191 days, with a median time to event of 663 days. Table 3 shows multivariable HR for new and severe damage. Black race associated with increased new damage (1.29 (1.21, 1.37)). Black (1.47 (1.37, 1.57)) and Asian race (1.31 (1.13, 1.52)) associated with increased severe damage events which persisted in the full model (Table 3d). In the ADI model (Table 3c), the most and second most disadvantaged (vs. least) ADI associated with statistically significantly increased severe damage and any damage, respectively (HR ~1.3 and ~1.21), but less in the full model. Hispanic ethnicity showed no association, except when controlling for race and ADI where severe damage was higher (1.54 (1.25, 1.90)). Across all models, older age and comorbidities associated with increased damage and severe damage. Female sex associated with decreased new and severe damage events in most models but was non-significant when controlled for race, ethnicity, and ADI.
Conclusion: This study is among the first to investigate how neighborhood disadvantage impacts SLE damage beyond race/ethnicity. Comparing most to least advantaged ADI groups in multivariable analysis suggested ~30% increased hazard of serious SLE damage events. This higher hazard was only by race/ethnicity in fully controlled models, consistent with prior data. Some ADI association remained for any damage. Findings urge further investigation of mechanisms driving outcome disparities.
To cite this abstract in AMA style:
Katz J, Yu A, Elwert F, Greenlee R, Gazeley D, Rosenthal A, Cormier J, Sutherland B, Parikh S, Jiang Y, Bartels C. New and Severe Damage in a Prevalent Lupus Cohort Through the Lens of Demographic and Neighborhood Disparities [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/new-and-severe-damage-in-a-prevalent-lupus-cohort-through-the-lens-of-demographic-and-neighborhood-disparities/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/new-and-severe-damage-in-a-prevalent-lupus-cohort-through-the-lens-of-demographic-and-neighborhood-disparities/