Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: The 2023 ACR/EULAR classification criteria (2023 AECC) for antiphospholipid syndrome (APS) were recently published. The new criteria require an entry criterion and employe a weight-additive system. The aim of this study was to assess the performance of the 2023 AECC for APS in a Mexican cohort.
Methods: We enrolled individuals aged 18 years or older with a clinical diagnosis of primary (PAPS) and secondary APS (SAPS), alongside a control group consisting of individuals with non-autoimmune thrombophilia. Follow-up was conducted at a tertiary care center in Mexico City, from 1990-2023. We conducted a retrospective cohort study, in which we reviewed the clinical records of included patients from the time of their diagnosis to their last outpatient visit. We evaluated the fulfillment of the 2023 AECC and the 2006 Sydney classification criteria (2006 SCC), and their performance comparing them with the clinical diagnosis made by experienced rheumatologists, considered as the gold standard criteria. Demographic, clinical and serological data were obtained. Additionally, we calculated the Global Anti-Phospholipid Syndrome Score (GAPSS) at baseline and the Damage Index for Antiphospholipid Syndrome (DIAPS) at the last follow-up.
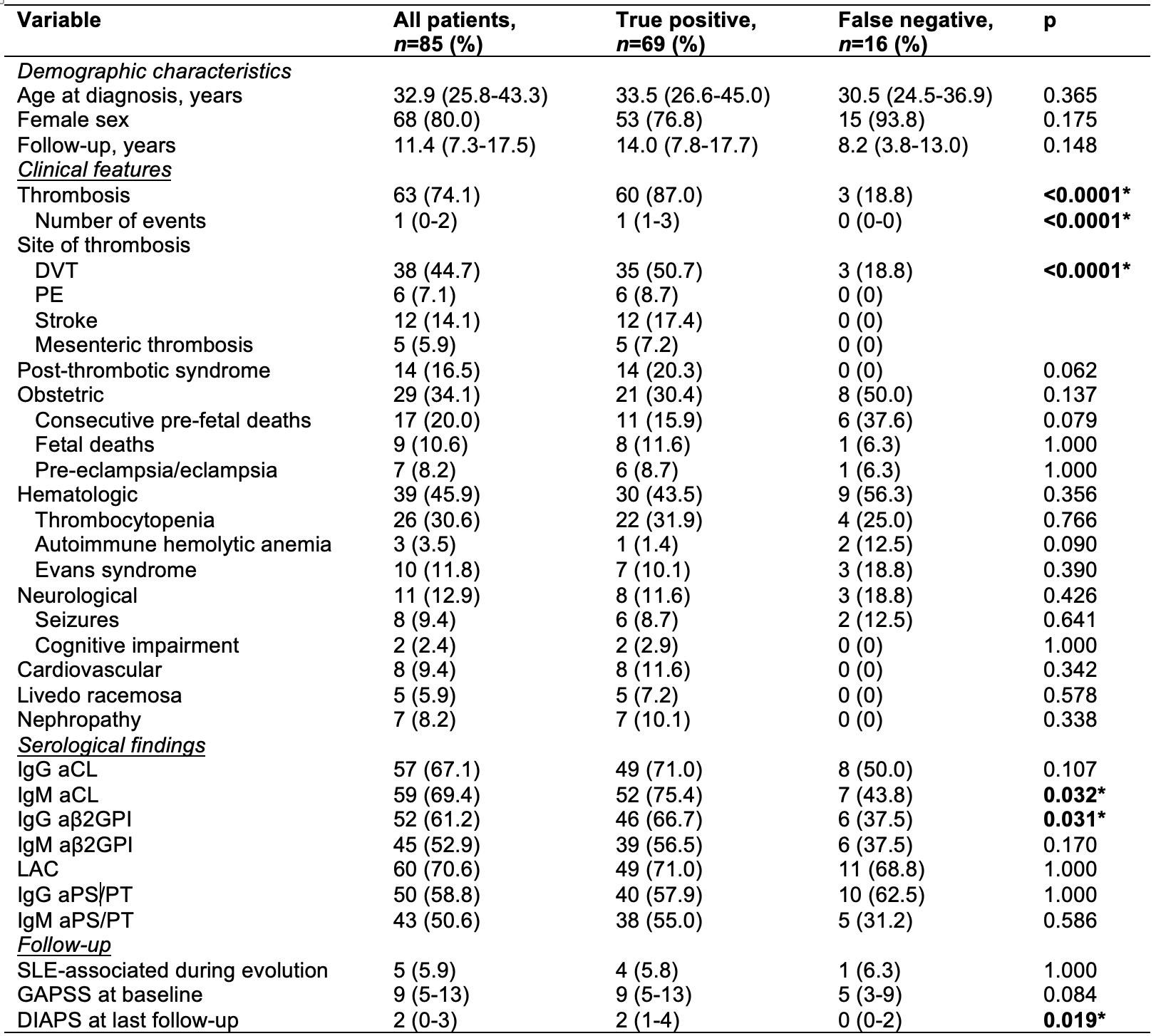
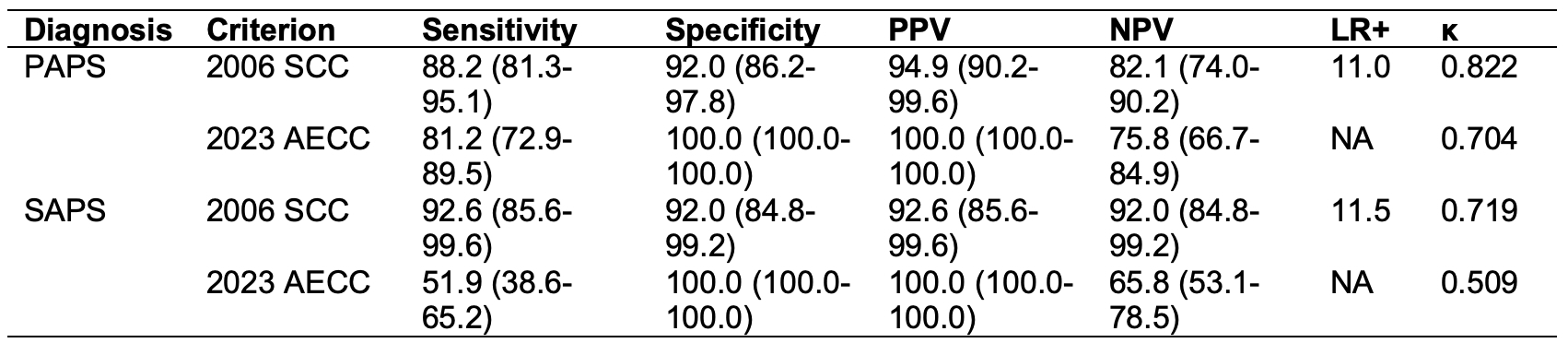
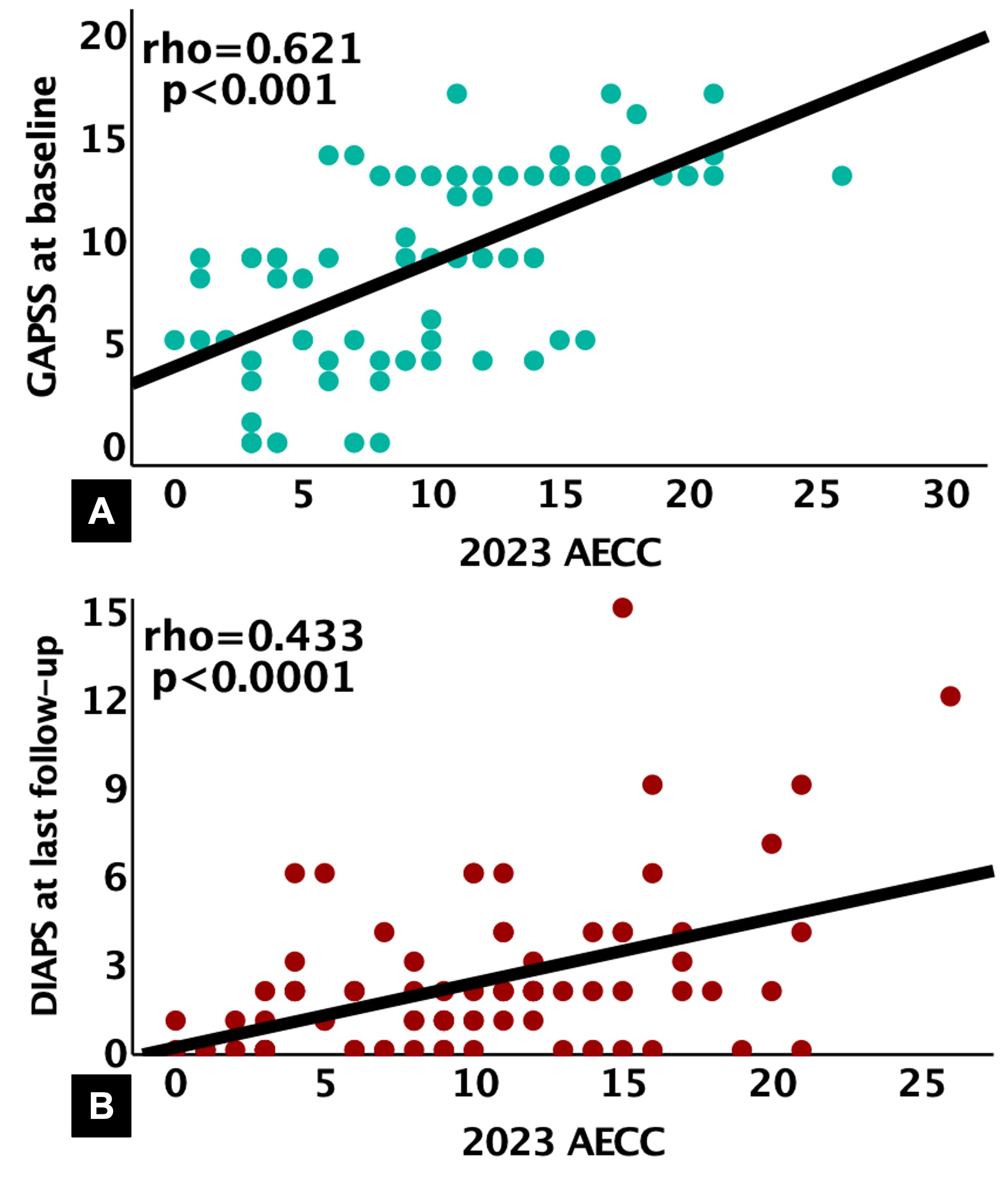
Results: We included 85 patients with PAPS, including 46 cases with only thrombotic, 12 cases with only obstetric manifestations and 8 cases of “pure” hematologic APS (recognized hematological APS feature plus serological Sydney criteria). There were also 54 patients with SAPS, associated with systemic lupus erythematosus (n=46), rheumatoid arthritis (n=4), Sjögren’s syndrome (n=2), Still’s disease (n=1), and systemic sclerosis (n=1). Furthermore, 50 patients with thrombophilia were included, comprising factor V Leiden (n=6), protein C (n=22), protein S (n=3), and antithrombin III deficiencies (n=5), and prothrombin (n=6) and MTHFR gene mutations (n=8). According to the 2023 AECC criteria, 69 (81.2%) patients with PAPS, 28 (51.9%) with SAPS, and none of the thrombophilia patients met the classification for APS. When comparing true positive (TP) (n=69) versus false negative (FN) (n=16) cases within the PAPS group, TP cases exhibited a higher frequency of thrombotic manifestations, IgM anti-cardiolipin (aCL) and IgG anti-β2-glycoprotein-I positivity (aβ2GPI) (Table 1). TP cases in PAPS exhibited a significantly higher DIAPS score (2 [IQR 1-4] vs. 0 [IQR 0-2], p=0.019) at the end of the follow-up period. For PAPS, a correlation was observed between the 2023 AECC score and baseline GAPSS (rho=0.621, p< 0.0001) and DIAPS at last follow-up (rho=0.433, p< 0.0001) scores (Figure 1). When comparing the 2023 AECC with the 2006 SCC, a lower sensitivity (81.2% vs. 88.2%) but a higher specificity (100.0% vs. 92.0%) was observed for PAPS. Similar findings were observed in SAPS. Furthermore, in both APS groups, the Cohen’s Kappa coefficient showed better agreement with the 2006 SCC (Table 2).
Conclusion: In both PAPS and SAPS, the 2023 AECC have higher specificity than the 2006 SCC. The main feature of PAPS patients according to the 2023 AECC was thrombosis, and these criteria might identify patients at higher risk of thrombosis and damage accrual.
Data are expressed as proportions (percentages) or medians (interquartile ranges). Statistical analysis: Chi-square or Fisher’s exact tests were used for nominal variables, the Wilcoxon rank-sum test was used for numerical variables.
DVT: deep vein thrombosis, PE: pulmonary embolism, aCL: anti-cardiolipin, aβ2GPI: anti-β2 glycoprotein I, LAC: lupus anticoagulant, aPS/PT: anti-phosphatidylserine/prothrombin complex, SLE: Systemic Lupus Erythematosus, GAPSS: Global Anti-Phospholipid Syndrome Score, DIAPS: Damage Index for Thrombotic Antiphospholipid Syndrome.
*Statistically significant between the true positive and false negative group comparisons.
Data are expressed as percentages (95% confidence intervals).
2006 Sydney classification criteria; 2023 American College of Rheumatology/European League Against Rheumatism classification criteria; PAPS: primary antiphospholipid syndrome; SAPS: secondary antiphospholipid syndrome; PPV: positive predictive value; NPV: negative predictive value; LR+: positive likelihood ratio, NA: not assessable; κ: Cohen’s Kappa coefficient
Correlations between 2023 AECC score and GAPSS score at baseline and DIAPS score at last of follow-up. A) 2023 AECC and GAPSS at baseline, B) 2023 AECC and DIAPS at last follow-up.
2023 AECC: 2023 ACR/EULAR Classification Criteria, GAPSS: Global Anti-Phospholipid Syndrome Score, DIAPS: Damage Index for Thrombotic Antiphospholipid Syndrome.
To cite this abstract in AMA style:
Cimé-Aké E, Hernández-Molina G, Llorente-Chávez A, Martin Nares E. Performance of the 2023 ACR/EULAR Classification Criteria for Antiphospholipid Syndrome in a Mexican Cohort [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/performance-of-the-2023-acr-eular-classification-criteria-for-antiphospholipid-syndrome-in-a-mexican-cohort/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/performance-of-the-2023-acr-eular-classification-criteria-for-antiphospholipid-syndrome-in-a-mexican-cohort/