Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: VEXAS syndrome is a recently-discovered systemic auto-inflammatory disease caused by somatic mutation at position 41 in the X-linked gene UBA1.1 First, 25 older men with M41T, M41V, or M41L with variant allele fraction (VAF) 35-80% were reported among quaternary referral populations of severely ill patients. A later study of 163,096 patients participating in a regional health system research cohort found 8 older men with the same UBA1 M41X mutations, with VAF 9-74%.2 Nearly all had severe anemia and macrocytosis, and five had a clinical diagnosis of VEXAS. This study population was >96% White and more than half of participants were >60 years old. Thus, there is a critical unmet need to define the prevalence and clinical consequences of somatic UBA1 M41L mutation in a racially and geographically diverse population.
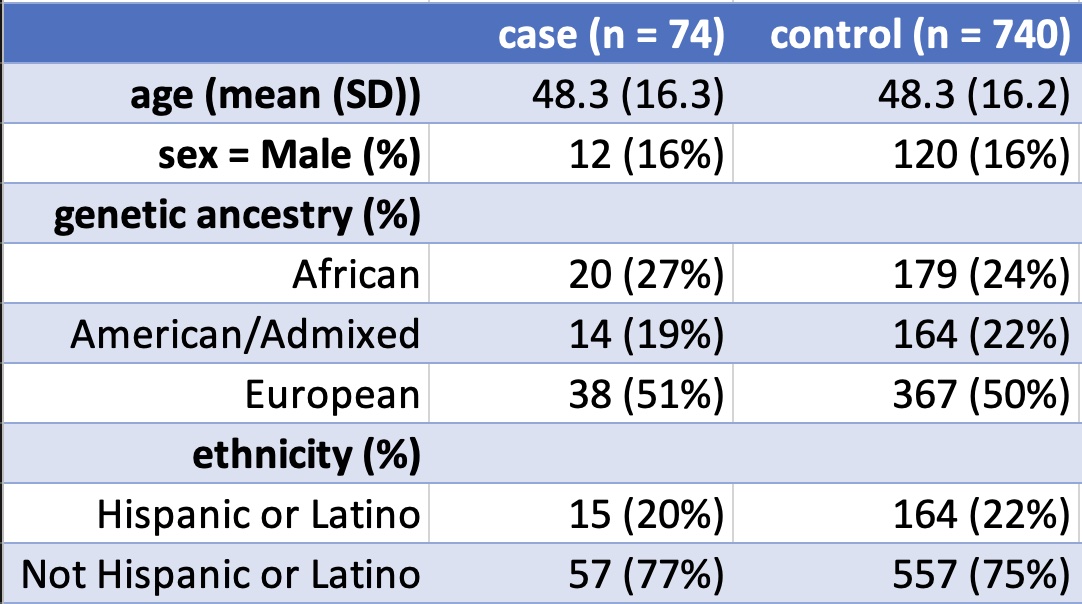
Methods: We analyzed 245,388 individuals with clinical-grade whole genome sequencing data in the NIH All of Us cohort v7 data release.3 Somatic variants in UBA1 were identified with Mutect2 4, annotated with Annovar 5, and filtered in R version 4.2.2 6 based on published pragmatic guidelines.7 VEXAS-associated SNOMED codes, laboratory abnormalities, and medications were defined by literature search of symptoms of confirmed cases.1,2,8 Controls were identified in a 10:1 ratio based on matching age and sex.
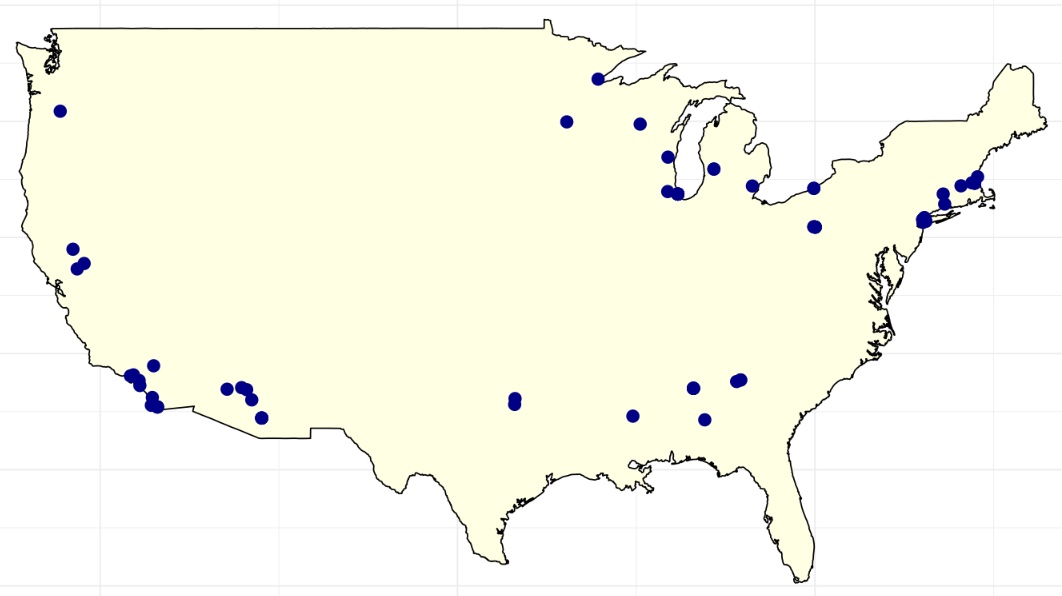
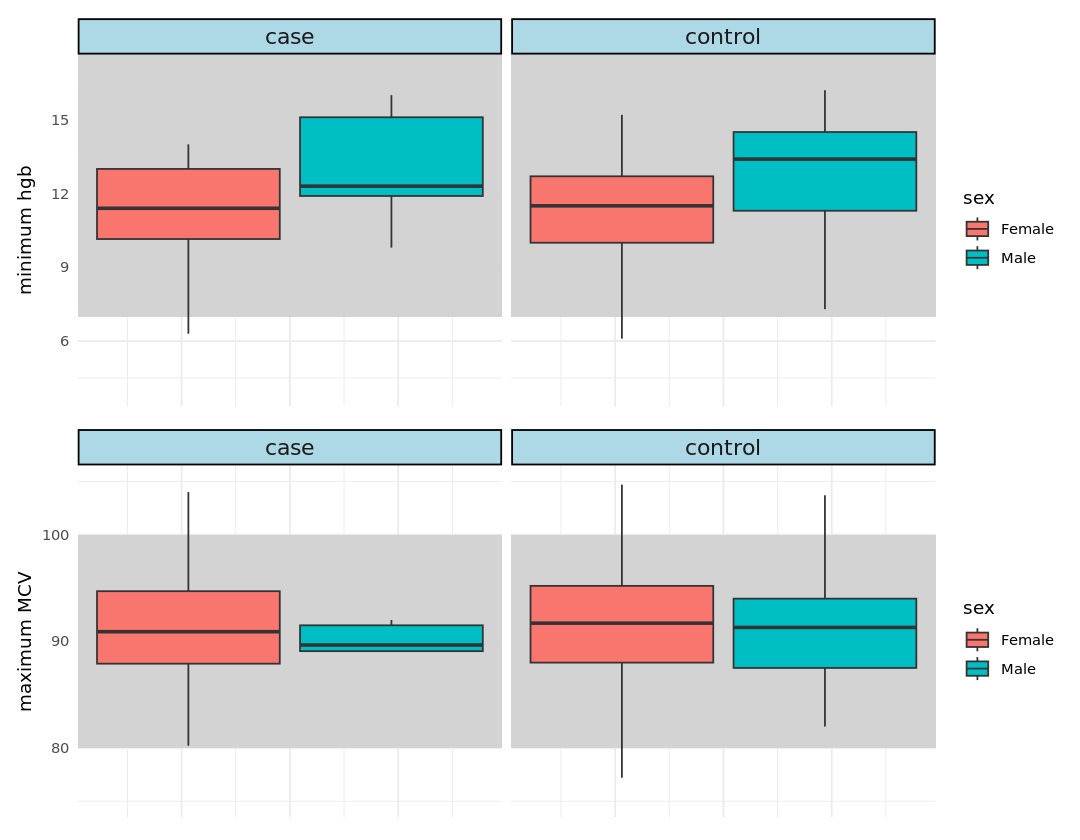
Results: 74 participants in the NIH All of Us cohort harbor somatic mutation UBA1 M41L and none have the other well-described variants, M41V or M41T. The M41L mutation was more common among women than men (n = 62 vs 12, p < 0.001) and no effect of age (p = 0.17) or ancestry (p > 0.4) was observed. The cases are age 20 to 83 and have VAF 4.5% to 33%. Their ancestry is 51% European, 27% African, and 19% admixed/Latino. The number of VEXAS-associated diagnosis codes was similar between cases and controls (4.3 vs 3.6, p = 0.77), but cases had an increased rate of asthma (27% vs 18%, p < 0.001), Tietze’s syndrome (8% vs 2%, p < 0.001), and neutropenia (7% vs 2%, p = 0.005). The minimum observed hemoglobin was similar between cases and controls (11.5 vs 11.4 mg/dL) as was the maximum mean corpuscular volume (91.7 vs 91.4). Interestingly, cases were much more likely to be prescribed systemic steroids than matched controls (55% vs 0%, p < 0.001).
Conclusion: We describe the largest cohort of people with somatic mutation M41L in the UBA1 gene and the largest cohort of women with a VEXAS-associated mutation. The diagnosis codes and laboratory values do not comport with the severe, systemic illness that has characterized our understanding of VEXAS to date. However, these cases were prescribed systemic steroids at a much higher rate than matched controls and are enriched for a few idiopathic inflammatory diagnoses suggesting an incompletely-appreciated inflammatory syndrome. These cases are younger, healthier, have lower VAF, and much better represent the demographic and geographic diversity of the United States than previous reports. We hypothesize that many of the cases reported here will not develop VEXAS due to either somatic reversion or haplosufficiency of UBA1. Further characterization of the genetic and clinical trajectories in these individuals may permit strategies for risk stratification, monitoring, and treatment.
To cite this abstract in AMA style:
Corty R, Bick A. Analysis of 245,388 Diverse Participants in the NIH All of Us Cohort Identifies VEXAS Resiliency in UBA1 M41L Somatic Mutation Carriers [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/analysis-of-245388-diverse-participants-in-the-nih-all-of-us-cohort-identifies-vexas-resiliency-in-uba1-m41l-somatic-mutation-carriers/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/analysis-of-245388-diverse-participants-in-the-nih-all-of-us-cohort-identifies-vexas-resiliency-in-uba1-m41l-somatic-mutation-carriers/