Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Depression is one of the most common neuropsychiatric disorders in patients with SLE. The Centre for Epidemiologic Studies Depression Scale (CES-D) has been used to determine depressive symptomatology with a score of 24 serving as the cut-off for depression in SLE. Instead of using this cut-off, we aimed to: 1) classify patients into one of two states representing being depressed or not using a hidden Markov model, and 2) identify socioeconomic factors that predict patients’ transition from a non-depressed state to a depressed state.
Methods: Data from the Lupus Outcomes Study at the University of California, San Francisco were analysed. Depressive symptoms were assessed with the CES-D annually providing up to 6 waves of observation. Patients with at least 2 waves of data were included. Under a Bayesian perspective, a contiguous-time hidden Markov model was fitted to the data, assuming that patients can be divided into two different states (non-depressed and depressed) over time. We assumed that CES-D scores follow a zero-inflated negative binomial distribution (excess of zeroes and integer outcome), and its means depend linearly on clinically relevant factors (Figure 2). Moreover, we included socioeconomic factors (below poverty line, employment and higher education) that could potentially be associated with the transition between the non-depressed and the depressed state.
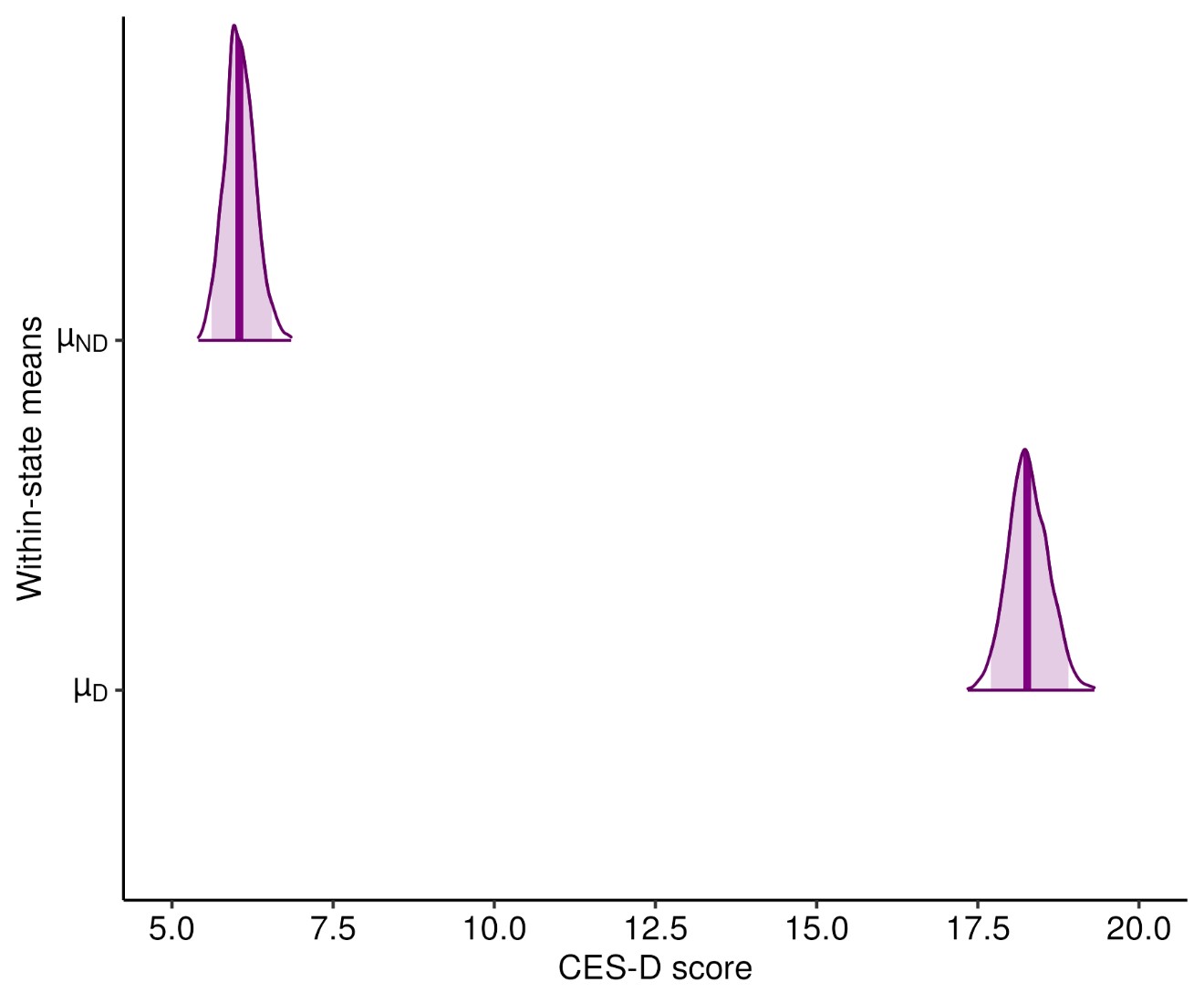
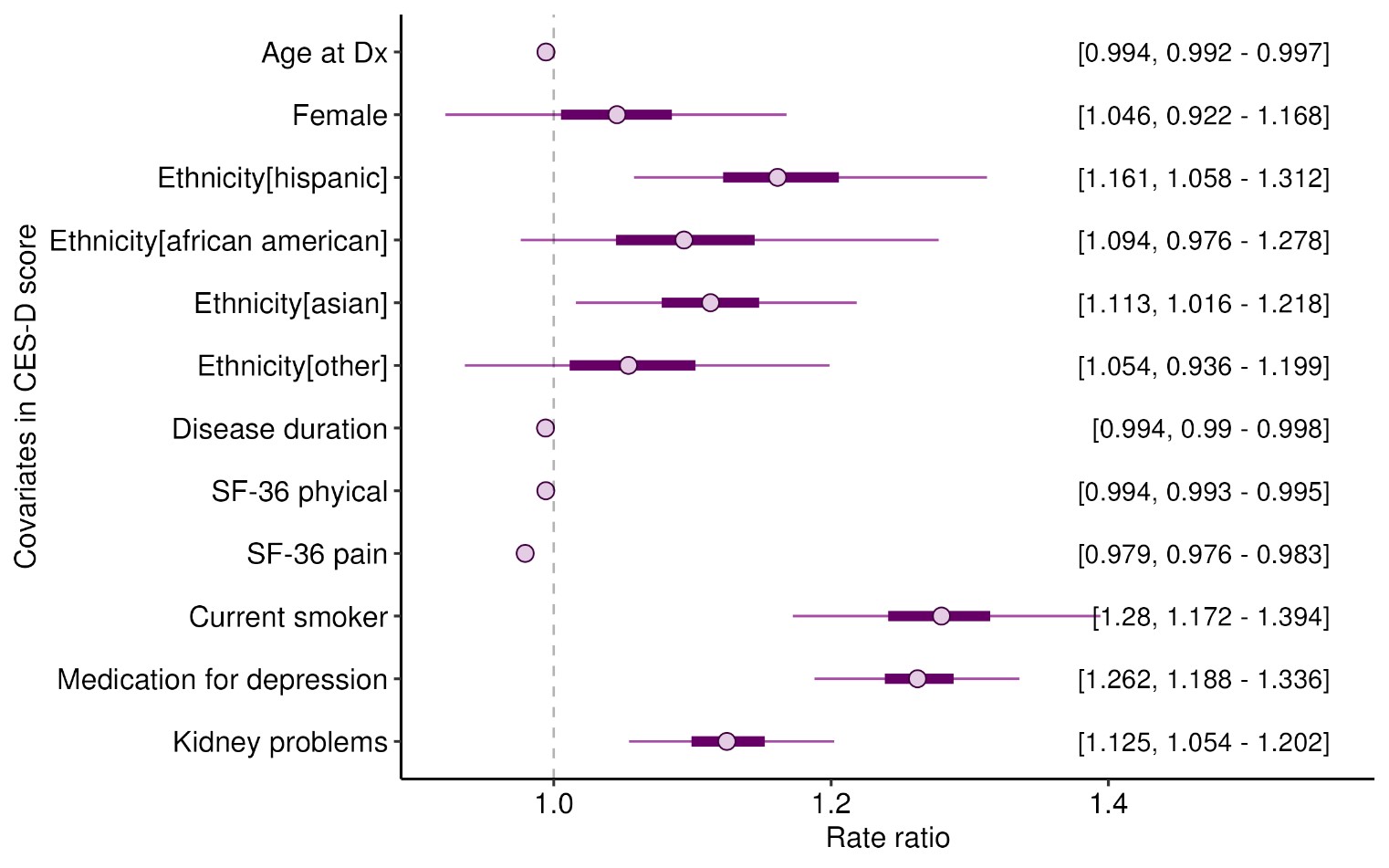
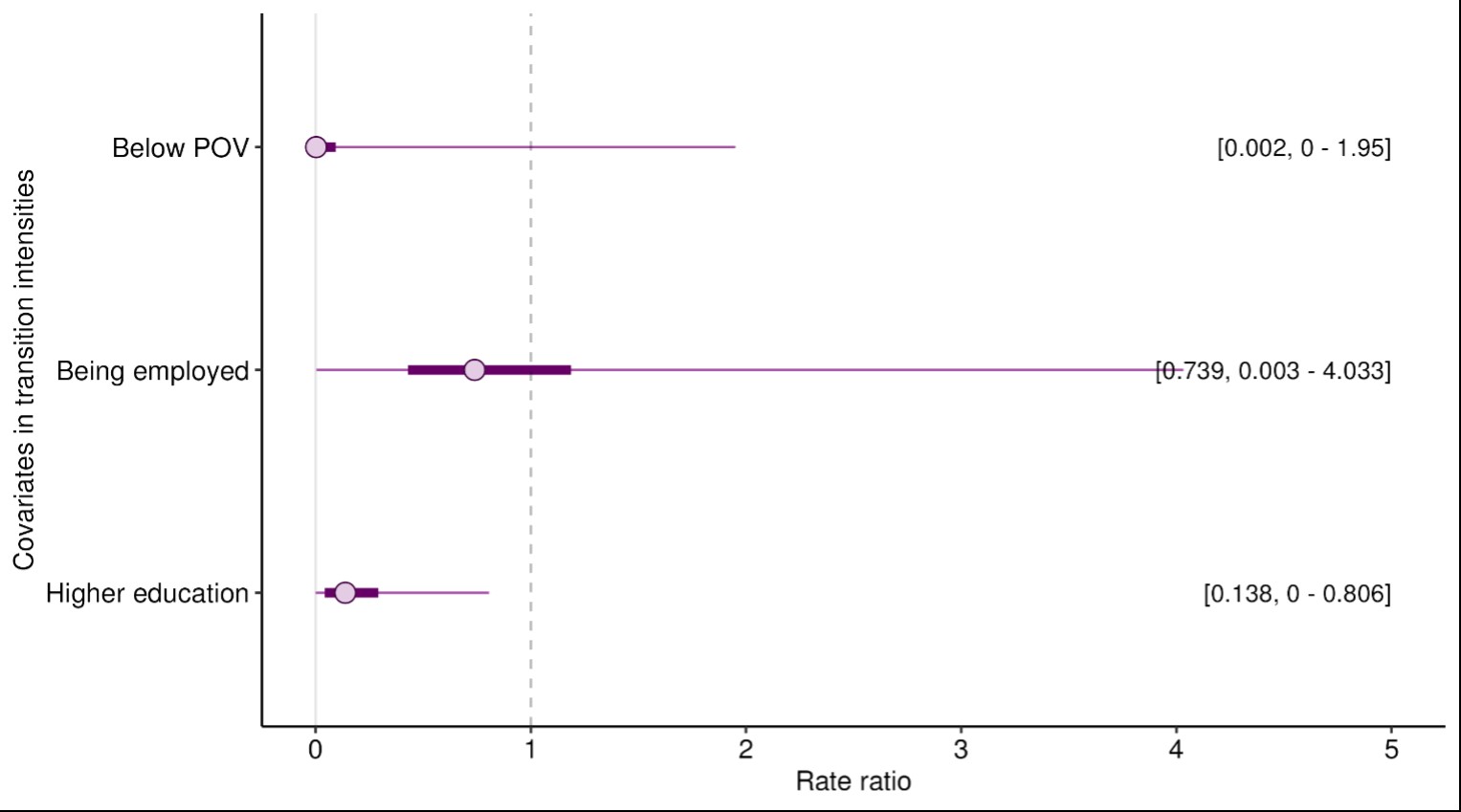
Results: 763 adults with SLE followed over 7 years were included. We found that the non-depressed state had a mean CES-D rate (μND) of 6.05 (95% CrI 5.61 – 6.55) whereas the depressed state mean rate (μD) was 18.3 (95% CrI 17.7 – 18.9) (Figure 1). The mean CES-D score rate decreased (improvement of depressive symptoms) by 2% for one-unit increase in SF-36 bodily pain score (higher scores means less pain), and it increased (worsening of depressive symptoms) by 12%, 26% and 28% for those with lupus related kidney disease, on anti-depressant, and current smokers versus those who did not smoke, respectively (Figure 2). Moreover, having higher education (college or more) decreased the rate of transitioning between the non-depressed state and the depressed state by 86% (Figure 3). For a patient who is not below the poverty line, nor employed and does not have higher education (i.e. transition covariates set to zero), the probability of transitioning between the non-depressed state and the depressed state was low (3%).
Conclusion: Using HMMs, we classified patients with SLE into two different states, depressed and non-depressed. Bodily pain, smoking, lupus related kidney disease and use of antidepressants drugs were associated with worsening depressive symptoms as measured by the CES-D. Transitioning between states was predicted by different factors over time, where higher education and employment significantly decreased the rate of transitioning between the non-depressed state and the depressed state.
X axis represents the distribution of the parameters of interest. Y axis represents the parameters where inference is made. The dark shaded region represents the point estimate from a frequentist point of view and the light shaded region represents the 95% uncertainty interval, i.e., with 95% of probability the estimate would lie in that region. As an example μ_ND represents the inference made on the unknown mean of the observed CES-D score given that it comes from the non-depressed state after adjusting for other clinical variables described in Figure 2.
X axis represents the rate ratio and Y axis represents the parameters where inference is made. For example, those who have kidney problems due to lupus have a 12.5% rate increase in their mean CES-D score compared to those without kidney problems. The dot on the graph represents the point estimate and the line represents the 95% CrI
X axis represents the hazard ratio and Y axis represents the parameters where inference is made. As an example, being below the POV had a protective effect (Rate ratio .002, 95% CrI 0 – 1.95), although this effect size was not significant. The dot on the graph represents the point estimate and the line represents the 95% CrI
To cite this abstract in AMA style:
Nariman Y, Diaz Martinez J, Bingham K, Katz P, Touma Z. Identifying SLE Patients with Depression Using a Zero-Inflated Hidden Markov Model and Predicting Factors Associated with Transition from a Non-depressed State to a Depressed State [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/identifying-sle-patients-with-depression-using-a-zero-inflated-hidden-markov-model-and-predicting-factors-associated-with-transition-from-a-non-depressed-state-to-a-depressed-state/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identifying-sle-patients-with-depression-using-a-zero-inflated-hidden-markov-model-and-predicting-factors-associated-with-transition-from-a-non-depressed-state-to-a-depressed-state/