Session Information
Date: Monday, November 13, 2023
Title: (1082–1099) Measures & Measurement of Healthcare Quality Poster I
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoporosis is a medical condition associated with decreased bone mass and bone architecture, which increases incidence of fragility fractures(4). It is associated with 1.5 million fractures in the United States annually and thus a major public health concern(1). Osteoporosis most often occurs in post-menopausal women; however autoimmune diseases and glucocorticoid treatment are also independent risk factors(2). Glucocorticoids remain the main treatment for giant cell arteritis (GCA) and polymyalgia rheumatica (PMR), and typically at high doses with an extended period of exposure. Prolonged use of glucocorticoids induces a low bone turnover state causing more pronounced impact on the synthesis rather than the resorption, leading to net loss of bone strength(5). Thus, high and prolonged doses of glucocorticoid treatment in GCA/PMR substantially increases the risk of fractures (3,5). Current guidelines for osteoporosis screening for patients on glucocorticoid treatment were published by the American College of Rheumatology (ACR). Nevertheless, rheumatologists and primary care providers often defer responsibility to one another or to other parties, leading to a lack of osteoporosis screening in GCA/PMR patients(5).This project aimed to increase the rate of ordering recommended screening for osteoporosis by at least 10% in patients diagnosed with GCA/PMR within the West Virginia University hospital system who have been treated with high dose glucocorticoids.
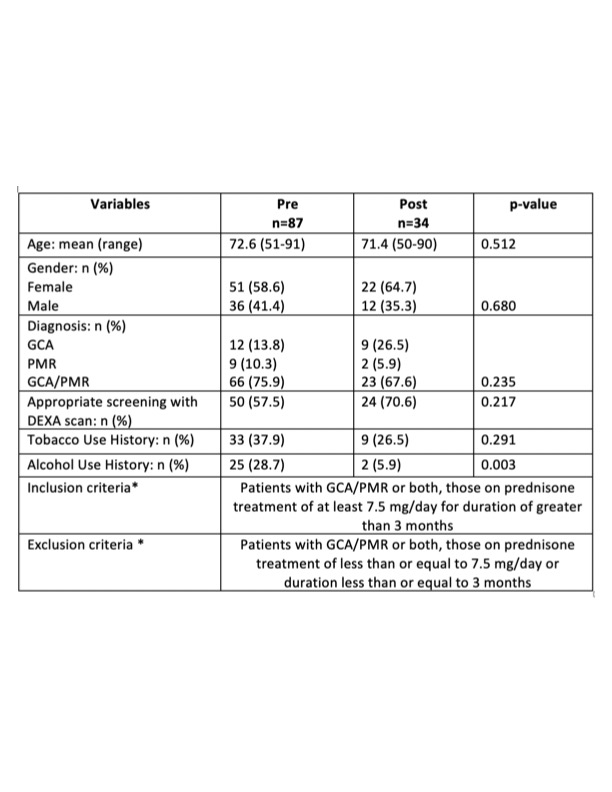
Methods: Patients (n=87) diagnosed with GCA/PMR and treated with high dose of glucocorticoids (≥ 7.5 mg of prednisone for greater than 3 months) were identified via chart review from 06/24/2020 to 12/13/2021. All patients with GCA/PMR included in our study met ACR diagnostic criteria. The number of DEXA scans ordered for patients diagnosed with GCA/PMR was measured pre-intervention. The PDSA (plan-do-study-act) model was then used to implement a quality improvement (QI) initiative at the provider level, which included provider education (email and verbal) coupled with an EPIC best practice alert for this specific patient population. The number of DEXA scans ordered was assessed two months after QI implementation in post-intervention patients (n=34).
Results: Only 57.5% of pre-intervention patients (n = 87, 72.6 ± 8.4 years old) had an appropriate screening completed with a DEXA scan. Within two months after QI implementation, the screening rate in post-intervention patients (n=34, 71.4 ± 9.2 years old) increased to 70.6% (p = 0.217).
Conclusion: Screening for osteoporosis is an important preventive measure for GCA/PMR patients, especially those on high doses of glucocorticoids. Our study demonstrates an improvement in DEXA screening rates by 13.1% over a period of two months by implementing reminders and education for providers in both rheumatology clinics and primary care clinics settings. Future implementation could be expanded at the patient level, through education and sending reminders to discuss the appropriateness of osteoporosis screening with their providers.
To cite this abstract in AMA style:
Tran K, Sockman E, Salyer R, Young M, Abbasi A, Verma D. Improving Osteoporosis Screening in Patients with Polymyalgia Rheumatica and Giant Cell Arteritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/improving-osteoporosis-screening-in-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-osteoporosis-screening-in-patients-with-polymyalgia-rheumatica-and-giant-cell-arteritis/