Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Acute myocardial infarction (AMI) can be divided into coronary artery disease (MICAD) or nonobstructive coronary arteries (MINOCA) according to the severity of artery stenosis on coronary angiography. Antiphospholipid syndrome (APS) can present with AMI, but the subtype and prognosis of these patients were not fully understood.
Methods: A single-center study was conducted based on the APS cohort in Peking Union Medical College Hospital. According to coronary angiography, AMI patients were classified as MICAD (≥50% stenosis) or MINOCA(<50% stenosis). Baseline and follow-up data were compared to identify differences between the two subgroups. Cox analysis was used to find prognostic factors associated with AMI recurrence.
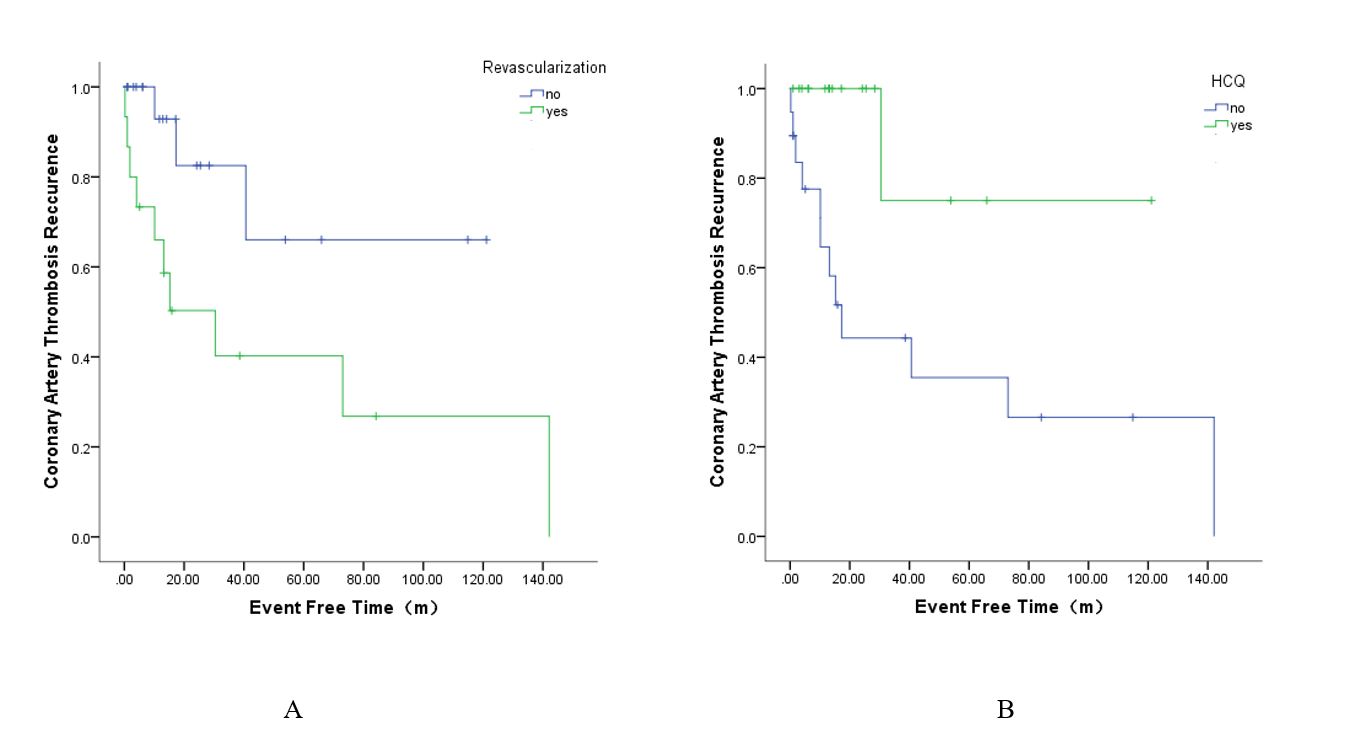
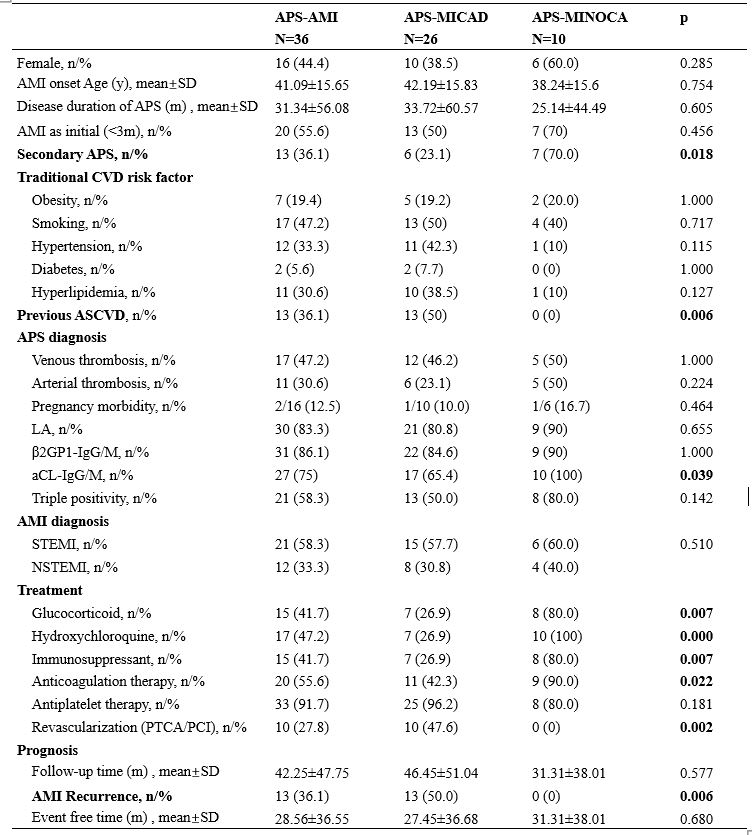
Results: The study enrolled 36 APS-AMI patients underwent coronary angiography, 26 (72%) patients were diagnosed with MICAD and 10 (28%) patients with MINOCA. Comparison between the two subgroups showed MINOCA patients were more likely to present in APS secondary to SLE than MICAD (70% VS 23.1%, p=0.018), and less likely to comorbid with previous atherosclerotic cardiovascular disease (ASCVD) (0 VS 50%, p=0.006). Anti-cardiolipin antibody (aCL) was more common in MINOCA (100% VS 65.4%, p=0.039). Treatment strategies were different, MINOCA patients tended to receive glucocorticoid (80% VS 26.9%, p=0.007), immunosuppressant (80% VS 26.9%, p=0.007), hydroxychloroquine (100% VS 26.9%, p=0.000) and anticoagulation (90% VS 42.3%, p=0.022), while MICAD patients were more likely to receive revascularization (47.6% VS 0%, p=0.002). 2 (5.5%) patients died and 13 (36.1%) patients experienced a relapse of AMI during a mean follow-up time of 42.25 months. Recurrence occurred only in MICAD group (13/26, 50%), over 60% (8/13) had recurrence more than once. Hydroxychloroquine was found to be a protective factor for AMI recurrence by Cox analysis [HR (hazard ratio) = 0.106, CI (confidence interval) = 0.014-0.823, p= 0.032], only 1 (5.8%) patient on hydroxychloroquine relapsed. While 66.7% (10/15) patients received revascularization suffered AMI recurrence caused by stent stenosis/thrombus, and the HR of recurrent AMI with revascularization therapy was 4.041 (CI = 1.087-15.021, p = 0.037).
Conclusion: APS AMI patients can be divided into two subgroups with different clinical and prognostic characteristics. Hydroxychloroquine can prevent relapse, while revascularization therapy has a high risk for AMI recurrence.
To cite this abstract in AMA style:
Curtis J, Gavigan K, Nowell W, Curtis D, Ali D, Liu X, Makaroff K, Almario C, Khalil C, Choi S, Spiegel B. The Subtype and Prognosis of Acute Myocardial Infarction in Antiphospholipid Syndrome Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/the-subtype-and-prognosis-of-acute-myocardial-infarction-in-antiphospholipid-syndrome-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/the-subtype-and-prognosis-of-acute-myocardial-infarction-in-antiphospholipid-syndrome-patients/