Session Information
Date: Monday, November 14, 2022
Title: SLE – Diagnosis, Manifestations, and Outcomes Poster III: Outcomes
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Multiple studies have documented that patients with SLE have a higher all-cause mortality. Active disease contributes to early deaths with later deaths more likely due to cardiovascular disease and malignancy. In this study we present the pattern of mortality in a single long-term, prospective cohort using death certificates to document cause of death.
Methods: The cohort consists of 2,238 patients (92% female, 52% Caucasian, 39% African-American) with 92% from Maryland and surrounding states (MD 71%, VA 9%, PA 7%, DE 3%, WV 1%, DC 1%). Death records for 1,288 patients lost to follow up prior to 2020 were obtained from the National Death Index (NDI) at the Center for Disease Control (Atlanta, GA). The NDI identified 11,369 death records from 1985 to 2019 as possible matches based on name, gender, race, and date of birth. Primary and secondary causes of death were provided for the best match for each patient. The causes of death were based on CDC classifications of ICD10 and ICD9 codes. Lupus was identified as a cause of death if ICD10 code M32.X or L93.0, or ICD9 code 695.X or 710.0 was listed on the death record.
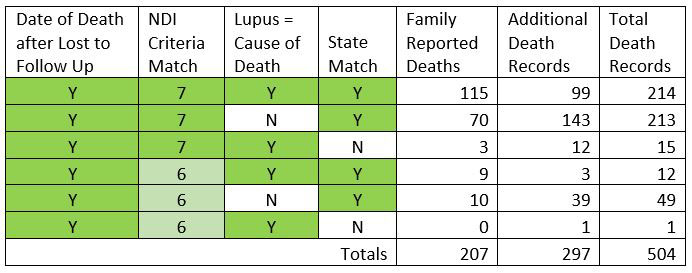
There were 207 death records identified by matching the NDI data elements and the date of death on the certificate to the date of death reported by the family. Analysis of these 207 records provided the following set of criteria that identified additional death records from the remaining 1,079 patients lost to follow up: 1) date of death occurred after the patient was lost to follow up; 2) at least six out of seven data elements sent to NDI matched those on the death record; and 3) EITHER lupus was listed as a cause of death on the death record OR the state of residence matched the state listed on the death record. Using these criteria, an additional 297 death records were found (Table 1).
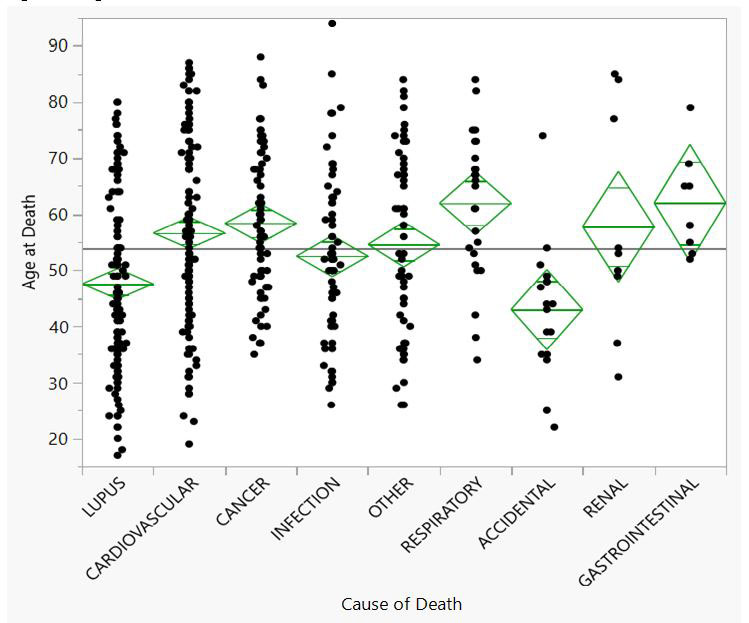
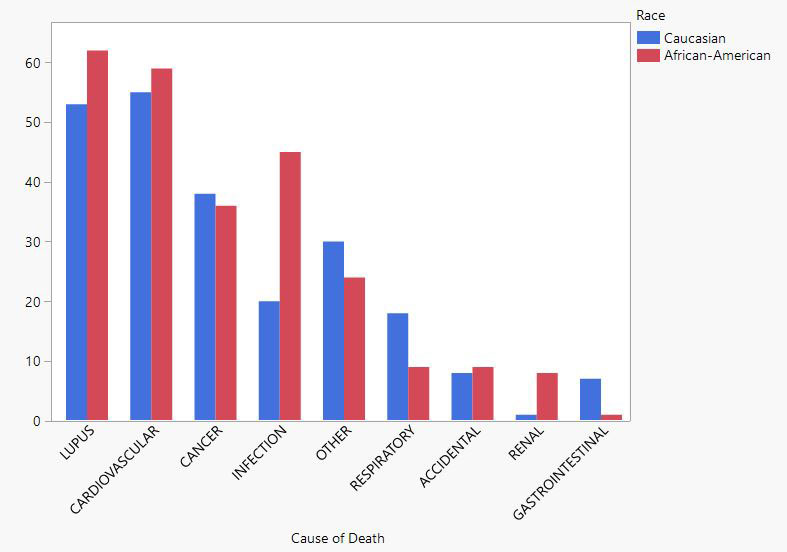
Results: The leading primary causes of death listed on the death certificate were: lupus (n=116, 23%), cardiovascular (n=114, 23%), cancer (n=74, 15%), infection (n=66, 13%), other (n=55, 11%), respiratory (n=28, 6%), accidental (n=17, 3%), renal (n=9, 2%) and gastrointestinal (n=8, 2%). Lupus deaths and accidental deaths occurred at a significantly younger age (p-values less than 0.05 for paired t-tests; Figure 1). African-Americans died at a younger age compared to Caucasians (50 ± 15 years vs 58 ± 16 years, p< 0.001). African-Americans had a higher proportion of deaths from infections and renal causes compared to Caucasians (p=0.0017 Likelihood ratio test; Figure 2).
Conclusion: SLE patients died at an average of 55 years of age for all causes of death (compared to life expectancies of >80 years for females in the US), with lupus and cardiovascular disease identified as the leading causes of death on death certificates. Cancer and infection were the third and fourth causes of death. African-Americans died younger than Caucasians and had more infection and renal causes of death. Only respiratory deaths were significantly more common in Caucasians.
To cite this abstract in AMA style:
Petri M, Levy J, Sbarigia U, Goldman D. All-Cause Mortality in a Systemic Lupus Erythematosus Cohort [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/all-cause-mortality-in-a-systemic-lupus-erythematosus-cohort/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/all-cause-mortality-in-a-systemic-lupus-erythematosus-cohort/